-
Články
Reklama
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
ReklamaMultiple Masses on the Tongue of a Patient with Generalized Mucocutaneous Lesions
article has not abstract
Published in the journal: . PLoS Med 5(11): e212. doi:10.1371/journal.pmed.0050212
Category: Learning Forum
doi: https://doi.org/10.1371/journal.pmed.0050212Summary
article has not abstract
Presentation of Case
In May 2007, a 62-year-old man presented with a 6-cm fungating mass on the dorsum of the tongue (Figure 1), which had lasted for an unknown period of time. The lesion had a roughened and irregular surface, with areas of white keratosis admixed with areas of necrosis. It felt indurated on palpation. Two additional smaller exophytic lesions were observed on the dorsum of the tongue: one adjacent to the main mass and the other on the apex. Both showed surface nodularity and minimal surface keratin production. The surrounding mucosa demonstrated hyperkeratosis and a pebbled surface. Interlacing white keratotic striae were observed on the right buccal mucosa (Figure 2), while the mucosa of the left cheek had an erosive area bordered by fine, white radiating striae (not shown in figure).
Fig. 1. The Dorsum of the Patient's Tongue 
On biopsy, the three exophytic masses turned out to be oral carcinomas, while the surrounding hyperkeratotic area showed histologic features of oral lichen planus. Fig. 2. Interlacing White Striae on the Right Buccal Mucosa, Consistent with the Diagnosis of Oral Lichen Planus 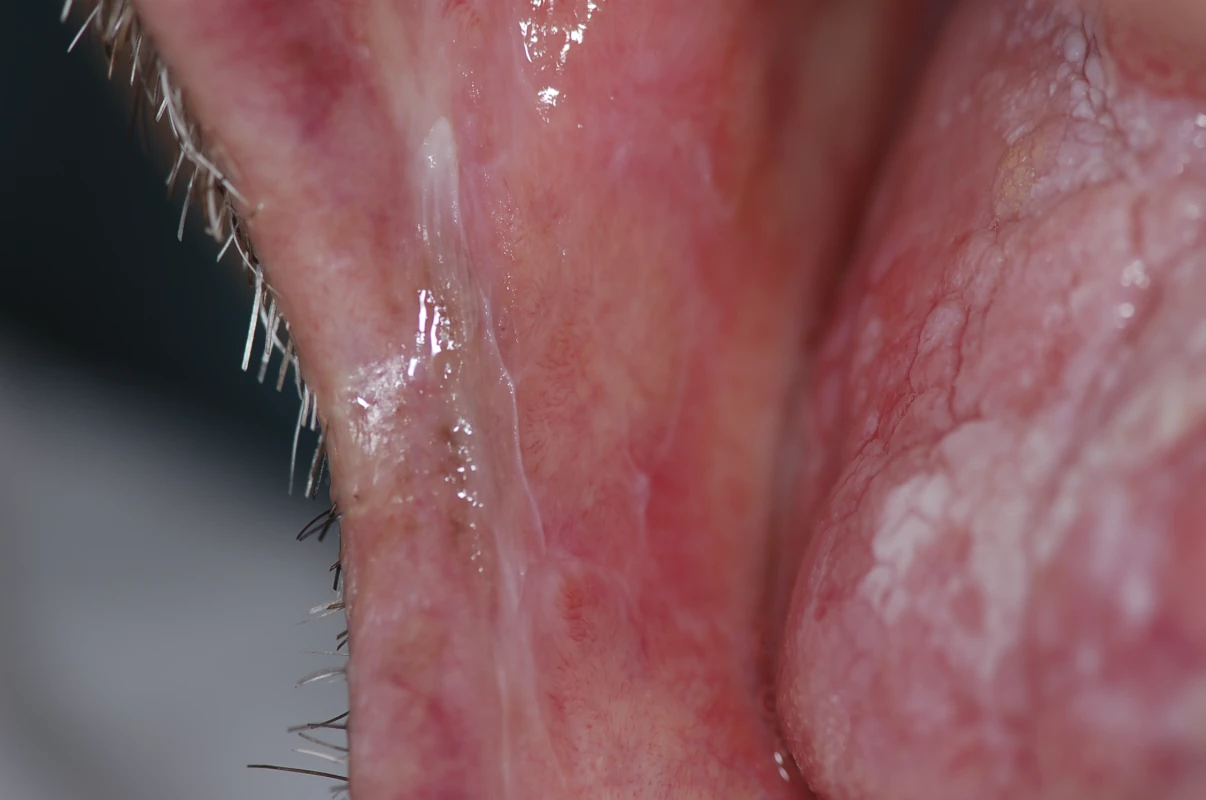
A skin examination revealed polygonal, flat-topped papules covered with a fine network of white lines on the legs (Figure 3). Furthermore, the patient had an erosive area on his glans penis (Figure 4).
Fig. 3. Polygonal, Flat-Topped Papules Covered with a Fine Network of White Lines on the Legs, Consistent with the Diagnosis of Lichen Planus 
Fig. 4. Erosive Area on the Glans Penis, Consistent with the Diagnosis of Lichen Planus 
What Clinical Diagnoses Were Considered?
The clinical appearance of the fungating mass immediately raised a high suspicion of malignancy, and a biopsy was promptly planned. For the two other exophytic lesions on the dorsum of the tongue, the differential diagnosis included squamous cell carcinoma, verrucous carcinoma, squamous papilloma, condyloma acuminatum, focal epithelial hyperplasia, and verruciform xanthoma.
The differential diagnosis of the hyperkeratotic surrounding area included plaque-like lichen planus, leukoplakia (thick or verruciform), proliferative verrucous leukoplakia, and lichenoid mucositis.
With regard to the buccal lesions, a clinical diagnosis of oral lichen planus (OLP) was relatively straightforward, given the presence of the bilateral interlacing white keratotic striae. Similarly, the skin lesions were highly suggestive of lichen planus, with the typical polygonal papules covered with a fine, lace-like network of white lines (so-called Wickham striae; in analogy, the interlacing white lines of reticular OLP are also referred to as Wickham striae by some authors).
The erosive area on the glans penis could be erosive lichen planus, pemphigus vulgaris, mucous membrane pemphigoid, plasma cell balanitis (or Zoon balanitis), or erythroplasia of Queyrat.
Progress
On biopsy, the fungating mass on the dorsum of the tongue showed features of an invasive squamous cell carcinoma, while the contiguous exophytic lesion turned out to be a verrucous carcinoma; the mass on the apex of the tongue was a squamous cell carcinoma in situ. Histologic appearance of the hyperkeratotic surrounding area was consistent with OLP.
Biopsies of either buccal and cutaneous lesions were not performed; nonetheless, both were diagnosed as lichen planus on the basis of the striking clinical findings alone. A biopsy of the genital lesion was not considered a priority at that time; in accordance with the concomitant oral and skin involvement, a presumptive diagnosis of erosive lichen planus was made.
Which Tests Would Now Be Helpful?
Once a biopsy-proven diagnosis of oral cancer is made, a staging workup is necessary in order to determine the extent of the primary tumor, the regional lymph node status, and the presence of distant metastasis. For this purpose, a comprehensive head and neck examination and imaging studies (computed tomography and/or magnetic resonance imaging; more recently, also positron emission tomography) are performed, and the cancer is staged according to the TNM (tumor, node, metastasis) system [1] (Tables 1 and 2). Depending on the clinical stage, location, and histologic findings of the primary cancer, general health status of the patient, and the patient's wishes, treatment of oral cancer is individually planned for each case.
Tab. 1. TNM Classification System for Oral Squamous Cell Carcinoma 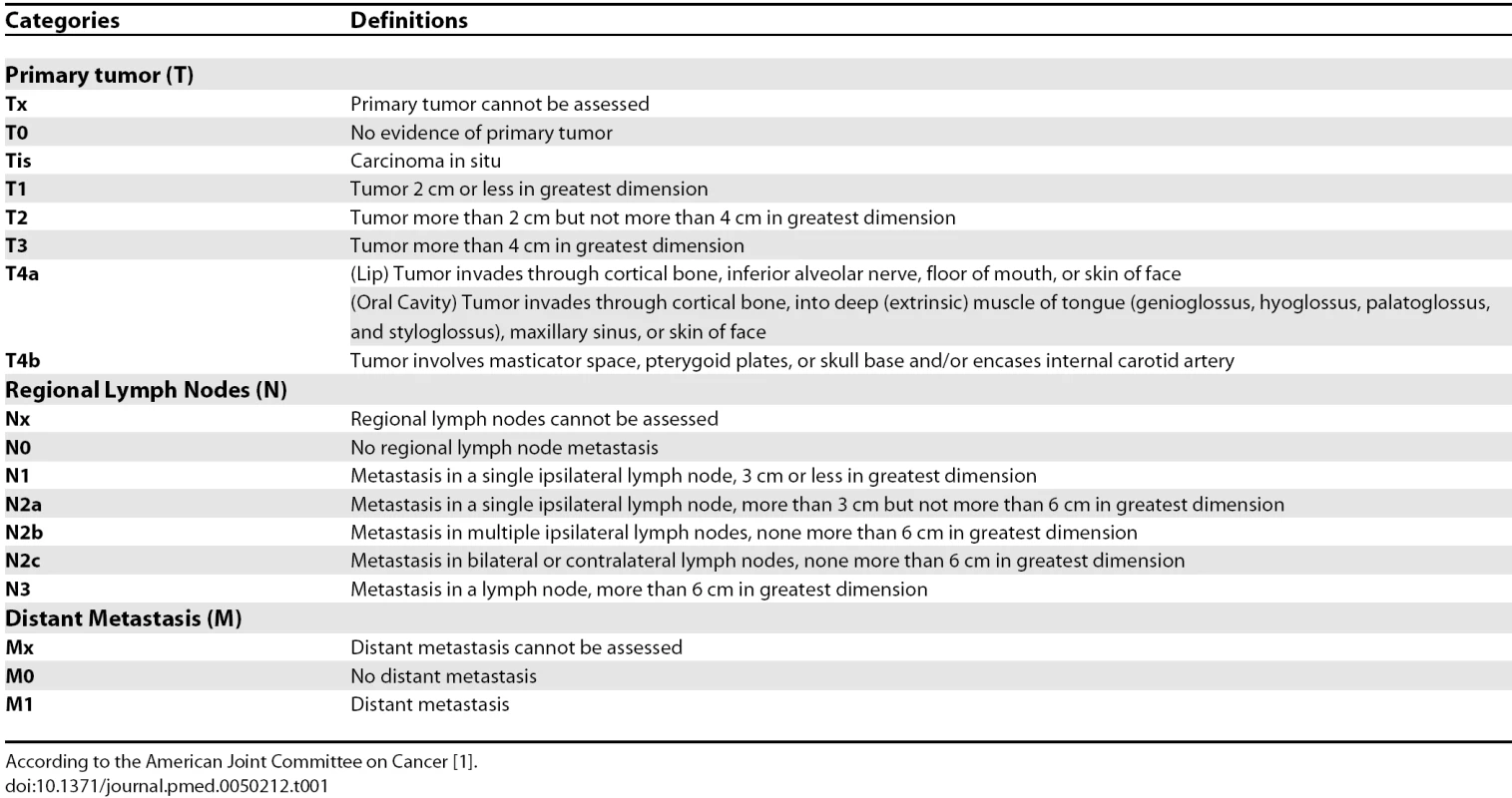
According to the American Joint Committee on Cancer [1]. Tab. 2. Stage Grouping 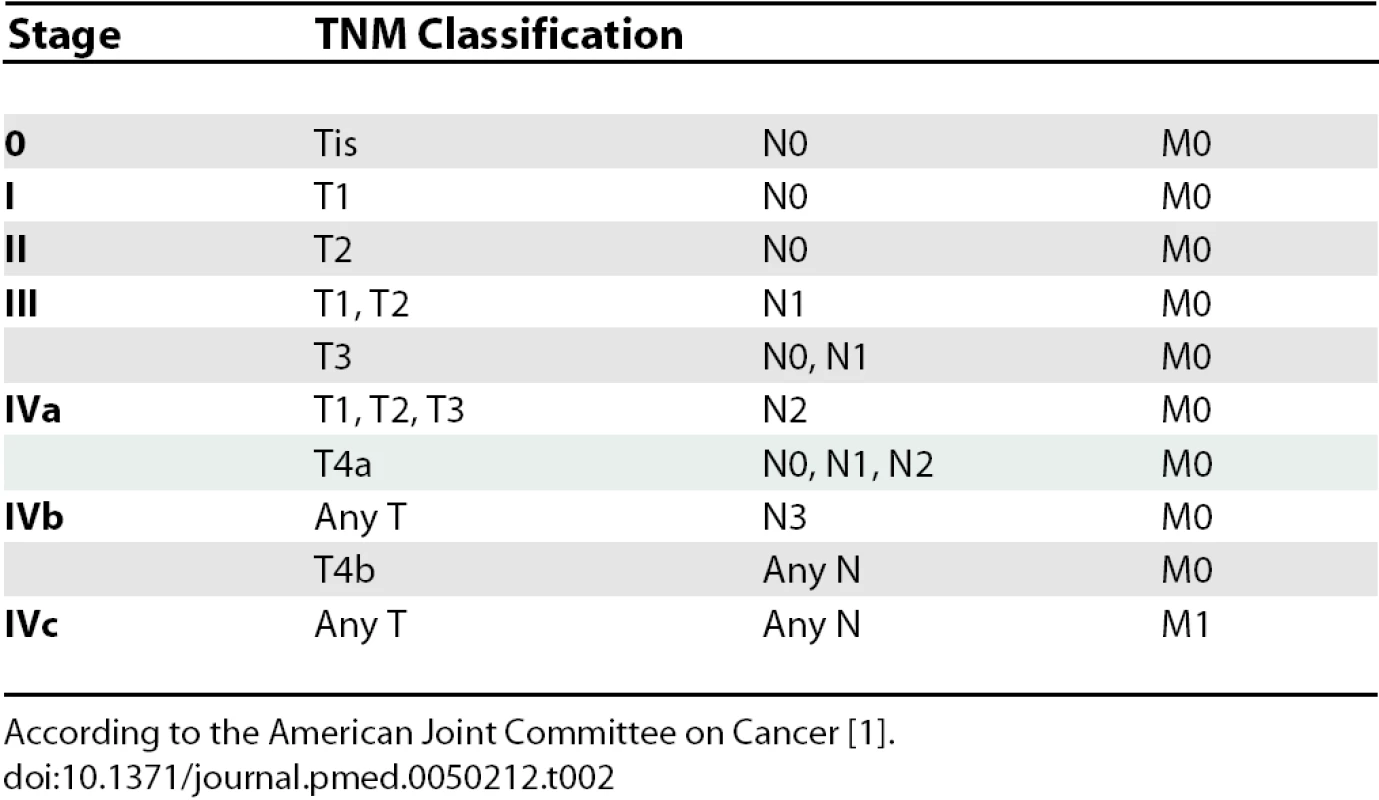
According to the American Joint Committee on Cancer [1]. In this patient, total-body computed tomographic scans revealed multiple enlarged lymph nodes in the left laterocervical and submandibular regions, while there was no evidence of distant metastasis. On the basis of clinical and imaging data, the invasive tumor was staged as T4 N2 M0.
Progress
The patient underwent surgery, with partial glossectomy and ipsilateral neck dissection. On histologic examination, the invasive cancer was identified as moderately differentiated squamous cell carcinoma that had widely invaded into muscles. Lymph node metastases were moderately differentiated squamous cell carcinomas as well, with no extracapsular extension. Based on additional data acquired from pathologic examination, the pathologic staging (pTNM) was T4a N2b M0 (stage IVa). Resection margins were free of tumor, and postoperative radiotherapy was given only on the neck.
The general health status of the patient rapidly worsened after surgery, and at a two-month follow-up evaluation a new mass was observed on the base of the tongue. On biopsy, this was diagnosed as a new squamous cell carcinoma, but a second surgical treatment was not planned, given the very poor health status of the patient. Combined radiotherapy and chemotherapy were prescribed, but the patient died two months later.
The family gave written consent for details of this case to be published.
Discussion
Oral cancer is a global health problem; worldwide, nearly 275,000 patients are annually estimated to have oral cancer, which represents about 3% of all malignancies in men and 2% in women [2]. The vast majority of oral cancers (approximately 94%) are squamous cell carcinomas that arise from the epithelium of the oral mucosa [3]. Survival of patients with oral cancer is directly related to the stage of disease at diagnosis; in fact, the five-year relative survival rate increased from 26.5% for oral cancers diagnosed at a distant stage to 81.8% for cases diagnosed at a localized stage [4]. Squamous cell carcinomas of the tongue seem to have lower rates of overall survival compared with cancers located in other oral cavity sites [5]. Unfortunately, only 33% of oral cancers are diagnosed at a localized stage, when the disease may be more easily and successfully treated [6]. This fact is responsible for a relatively poor overall five-year survival rate (59.1%), which has not significantly improved in the past several decades [6]. As a consequence, early detection is critical to reduce oral cancer mortality. In 9% to 25% of patients with oral cancer, additional synchronous or metachronous primary oral or pharynx carcinomas develop [3]; for these patients, the survival rates are worse.
Current therapeutic options for oral cancer include surgery, radiotherapy, and chemotherapy (each alone or in various combinations). In general, a wide surgical excision of the primary tumor remains the first line of treatment, even though stage I and stage II oral cancers could also be successfully treated with radiotherapy alone [7]. For stage III and stage IV oral cancers, surgery may be combined with radiotherapy and/or chemotherapy. A postoperative radiotherapy leads to better outcomes than radiotherapy administered preoperatively [8]. Indications for a postoperative radiation therapy include: positive surgical resection margins, bone or perineural invasion, multiple positive lymph nodes, or extracapsular lymph node invasion [9].
Chemotherapy can be given before surgery, after surgery and before radiotherapy, at the same time as radiotherapy, or alternating with radiotherapy. There is some evidence that postoperative concurrent radiotherapy and chemotherapy are more effective than postoperative radiotherapy alone in patients with advanced oral cancers [10], although this combined treatment may increase complications [11]. When there is clinical and/or imaging evidence of cervical lymph node metastasis, a neck dissection is required. Elective selective neck dissection may be performed in the node-negative neck, given the possibility of occult neck lymphadenopathy. Size and location of the primary lesion, thickness of the tumor, and invasion of neural, vascular, or lymphatic structures are factors used to evaluate the risk of occult cervical metastasis [12].
However, primary prevention and early diagnosis remain the cornerstones of strategies for reducing oral cancer mortality. With regard to primary prevention, public education efforts must be made to encourage people to avoid high-risk behaviors, with tobacco smoking and alcohol consumption being the major risk factors. As to early detection, the American Cancer Society recommends a periodic cancer-related check-up, which should include examination for oral cancers [13], and guidelines for visual inspection of the oral cavity were suggested [14]. However, a recent Cochrane review concluded that there is insufficient evidence to recommend screening of the general population for oral cancer using visual examination or adjunctive tools (toluidine blue, brush biopsy, fluorescence imaging) as an effective method for decreasing oral cancer mortality [15]. Nonetheless, the authors recommended regular screening by visual inspection applied by qualified health care providers for high-risk groups [15]. Patients with potentially malignant disorders of the oral mucosa have an increased risk of development of oral cancer; for these patients, close monitoring is recommended [16].
Lichen planus is an immune-mediated chronic inflammatory disease that commonly affects the epithelium of the oral mucosa with a spectrum of clinical conditions, including keratotic, atrophic, erosive, and ulcerative lesions; epithelia of other sites can be involved, namely the skin, the glans penis, the vaginal and vulvar mucosa, and the scalp [17]. A simultaneous involvement of more than one mucocutaneous site occurs in a relatively high percentage of patients with lichen planus [18].
A number of studies have indicated that OLP may be a precancerous lesion, with reported rates of malignant transformation that range from 0.4% to 5.6% [19]. Nevertheless, the precancer character of OLP remains highly controversial; the criticism is largely based on the vagueness of the criteria used in many studies for the diagnosis of OLP [19]. It has been argued that a transformation rate of even 1% would imply that nearly all oral cancers would develop from OLP, which is actually unlikely [20]. Moreover, applying strict diagnostic criteria, a recent study found that only oral lichenoid lesions and not OLP are associated with an increased risk of malignant transformation [19], although it is important to note that the concept of oral lichenoid lesion is somewhat controversial as well [18]; at any rate, the authors do not advise monitoring of patients with OLP [19]. In addition, at present there are no data to demonstrate the effectiveness of long-term follow-up of patients with OLP in reducing morbidity and mortality from oral cancer [21]. Therefore, to date we have no robust evidence to support the hypothesis of a malignant potential of OLP, and evidence to justify a continuous recall of patients with this oral ailment is lacking as well.
In spite of this, our report should alert physicians and dental practitioners that a potential of malignant transformation of OLP presumably exists, although its actual magnitude is yet to be established. Two other worrying facts should be taken into account: a study of 2,071 patients with cutaneous lichen planus, with no information about the oral status, reported no increase in risk of skin cancer, while the risk of oral cancer was 5.9-fold increased [22]; another study involving patients with OLP who subsequently had one oral carcinoma found that additional synchronous or metachronous mouth malignancies developed in 56% of participants [23].
Key Learning Points
-
Oral cancer is a global health problem with a relatively poor prognosis, mainly due to late diagnosis; as a consequence, early detection is critical to reduce mortality.
-
There is insufficient evidence to support the effectiveness of current screening methods in decreasing oral cancer mortality; however, close monitoring of patients with potentially malignant disorders of the oral mucosa is recommended.
-
There is ongoing controversy as to the potentially malignant nature of oral lichen planus, and there is insufficient evidence to support the effectiveness of long-term monitoring of patients with oral lichen planus in reducing morbidity and mortality of oral cancer.
-
This report should alert physicians and dental practitioners that a potential of malignant transformation of oral lichen planus presumably exists, although its actual magnitude is yet to be established.
-
Well-powered prospective studies are needed to provide the highest levels of evidence for practice; in the meantime, long-term monitoring of patients with oral lichen planus should be advisable.
There is no doubt that further well-designed and well-powered long-term prospective studies, with validated diagnostic criteria for OLP, are needed to provide the highest levels of evidence for practice; in the meantime, long-term monitoring of patients with OLP should be advisable. The presence of generalized, mucocutaneous lesions could be a matter of greater concern.
Zdroje
1. American Joint Committee on Cancer
2006
AJCC Cancer staging atlas
New York
Springer-Verlag
19
26
2. FerlayJBrayFPisaniPParkinDM
2004
Globocan 2002: Cancer incidence, mortality and prevalence worldwide. IARC Cancer Base No. 5 version 2.0
Lyon
IARC Press
3. NevilleBWDammDDAllenCMBouquotJ
2002
Oral and maxillofacial pathology
2nd edition
Philadelphia
Saunders
356
367
4. RiesLAGMelbertDKrapchoMMariottoAMillerBA
2007
SEER Cancer Statistics Review, 1975–2004.
Available: http://seer.cancer.gov/csr/1975_2004/. Accessed 8 October 2008
5. RusthovenKBallonoffARabenDChenC
2008
Poor prognosis in patients with stage I and II oral tongue squamous cell carcinoma.
Cancer
112
345
351
6. JemalASiegelRWardEMurrayTXuJ
2007
Cancer statistics, 2007.
CA Cancer J Clin
57
43
66
7. DayTADavisBKGillespieMBJoeJKKibbeyM
2003
Oral cancer treatment.
Curr Treat Options Oncol
4
27
41
8. FanucchiMKhuriFDShinDJohnstonePASChenA
2006
Update in the management of head and neck cancer.
Update Cancer Ther
1
211
219
9. CarlsonE
2003
Surgical management of squamous cell carcinoma of the oral cavity.
In
RegeziJASciubbaJJJordanRCK
editors
Oral pathology—Clinical pathological correlations
4th edition
St. Louis
Saunders
61
63
10. OliverRJClarksonJEConwayDIGlennyAMacluskeyM
2007
Interventions for the treatment of oral and oropharyngeal cancers: Surgical treatment.
Cochrane Database Syst Rev 2007
00006205
11. CooperJSPajakTFForastiereAAJacobsJCampbellBH
2004
Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck.
N Engl J Med
350
1937
1944
12. CapoteAEscorialVMuñoz-GuerraMFRodríguez-CampoFJGamalloC
2007
Elective neck dissection in early-stage oral squamous cell carcinoma—Does it influence recurrence and survival.
Head Neck
29
3
11
13. SmithRACokkinidesVEyreHJ
2007
Cancer screening in the United States, 2007: A review of current guidelines, practices, and prospects.
CA Cancer J Clin
57
90
104
14. National Institute of Dental and Craniofacial Research
2001
Perform a death-defying act. The 90-second oral cancer examination.
J Am Dent Assoc
132
36S
40S
15. KujanOGlennyAMOliverRJThakkerNSloanP
2006
Screening programmes for the early detection and prevention of oral cancer.
Cochrane Database Syst Rev 2006
CD004150
16. HsueSSWangWCChenCHLinCCChenYK
2007
Malignant transformation in 1458 patients with potentially malignant oral mucosal disorders: A follow-up study based in a Taiwanese hospital.
J Oral Pathol Med
36
25
29
17. Al-HashimiISchifterMLockhartPBWrayDBrennanM
2007
Oral lichen planus and oral lichenoid lesions: Diagnostic and therapeutic considerations.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod
103
S25.e1
S25.e12
18. EisenDCarrozzoMBagan SebastianJVThongprasomK
2005
Oral lichen planus: Clinical features and management.
Oral Dis
11
338
349
19. van der MeijEHMastHvan der WaalI
2007
The possible premalignant character of oral lichen planus and oral lichenoid lesions: A prospective five-year follow-up study of 192 patients.
Oral Oncol
43
742
748
20. van der MeijEHSchepmanKPSmeeleLEvan der WalJEBezemerPD
1999
A review of the recent literature regarding malignant transformation of oral lichen planus.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod
88
307
310
21. MattssonUJontellMHolmstrupP
2002
Oral lichen planus and malignant transformation: Is a recall of patients justified.
Crit Rev Oral Biol Med
13
390
396
22. SigurgeirssonBLindelofB
1991
Lichen planus and malignancy. An epidemiologic study of 2071 patients and a review of the literature.
Arch Dermatol
127
1684
1688
23. MignognaMDFedeleSLo RussoLMignognaCde RosaG
2007
Field cancerization in oral lichen planus.
Eur J Surg Oncol
33
383
389
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2008 Číslo 11- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Nutraceutikum Armolipid Plus podle klinických důkazů zlepšuje lipidový profil − metaanalýza
- Snižuje terapie betablokátory kardiovaskulární benefit aerobního cvičení u pacientů s arteriální hypertenzí?
-
Všechny články tohoto čísla
- Multiple Masses on the Tongue of a Patient with Generalized Mucocutaneous Lesions
- Reporting Bias in Drug Trials Submitted to the Food and Drug Administration: Review of Publication and Presentation
- A Prospective Study of Spatial Clusters Gives Valuable Insights into Dengue Transmission
- Estimating the Global Burden of Snakebite Can Help To Improve Management
- Informed Consent and Shared Decision-Making: A Requirement to Disclose to Patients Off-Label Prescriptions
- Comparing Highly Efficacious Antimalarial Drugs
- Approaches to Sex Education: Peer-Led or Teacher-Led?
- Bias, Spin, and Misreporting: Time for Full Access to Trial Protocols and Results
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Multiple Masses on the Tongue of a Patient with Generalized Mucocutaneous Lesions
- Informed Consent and Shared Decision-Making: A Requirement to Disclose to Patients Off-Label Prescriptions
- Estimating the Global Burden of Snakebite Can Help To Improve Management
- Reporting Bias in Drug Trials Submitted to the Food and Drug Administration: Review of Publication and Presentation
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



