-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaEvidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
article has not abstract
Published in the journal: . PLoS Med 8(11): e32767. doi:10.1371/journal.pmed.1001122
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001122Summary
article has not abstract
Summary Points
-
The treatment gap for mental, neurological, and substance use (MNS) disorders is more than 75% in many low - and middle-income countries.
-
In order to reduce the gap, the World Health Organization (WHO) has developed a model intervention guide within its Mental Health Gap Action Programme (mhGAP).
-
The model intervention guide provides evidence-based recommendations developed with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology.
-
This article presents the management recommendations for MNS disorders, with a link to the World Health Organization website where all the background material may be accessed.
-
To our knowledge, this is a first exercise involving such an extensive and systematic evaluation of evidence in this area.
Why Evidence-Based Guidelines Are Urgently Needed
Mental, neurological, and substance use (MNS) disorders are highly prevalent and are responsible for 14% of the global burden of disease expressed in disability-adjusted life years (DALYs) [1]. The resources that have been provided in countries to tackle the huge burden are insufficient, inequitably distributed, and inefficiently used, which results in a large majority of people with these disorders receiving no care at all [2]–[7]. Even when available, treatment and care often is neither evidence-based nor of high quality. The result is a large treatment gap, with more than 75% in many low - and middle-income countries (LAMIC).
In order to reduce the gap, the World Health Organization (WHO) launched the Mental Health Gap Action Programme (mhGAP) to scale up services for people with MNS disorders, especially in LAMIC [1]. One essential component of mhGAP is to develop management recommendations (guidelines) for MNS disorders identified as conditions of high priority. The priority conditions included are depression, psychosis, bipolar disorders, epilepsy, developmental and behavioural disorders in children and adolescents, dementia, alcohol use disorders, drug use disorders, and self-harm/suicide. The priority conditions were selected because they represent a large burden [8] in terms of mortality, morbidity, or disability, have high economic costs, and are often associated with violations of human rights.
Evidence suggests that explicit, evidence-based, cost-effective packages of interventions can improve the processes and outcomes of health care when appropriately implemented. A package approach is being considered for a wide variety of health challenges such as the packages of interventions for family planning, safe abortion care, and maternal, newborn, and child health [9]. The recent grand challenges in global mental health underline the fact that all interventions should be evidence-based to provide programme planners, clinicians, and policy-makers with effective care packages [10]. While examples of evidence-based packages of care for MNS disorders exist that focus mainly on delivery mechanisms, they did not systematically synthesize and appraise the evidence base for interventions [11]. WHO therefore established a Guideline Development Group (GDG) in 2008 to develop evidence-based recommendations that adhered to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) principles for developing transparent, evidence-based WHO guidelines [12].
This article presents the management recommendations for MNS conditions, with a specific link (below) to the WHO website where all the background material may be accessed, including the evidence profiles and GRADE tables. Disseminating the recommendations through the scientific literature is important to generate feedback from health care professionals, policy–makers, and scientists. This will be helpful for re-defining the challenges (we may have omitted some important topics, or we should have addressed some other topics in a different way); re-evaluating the synthesized evidence; re-directing the development of the intervention guide for use in LAMIC; and re-defining any implementation strategies in LAMIC (Figure 1). In this article, we use the term “mental health” as a convenient label for MNS disorders.
Fig. 1. Steps in the formulation and implementation of the <i>mhGAP Intervention Guide</i>. 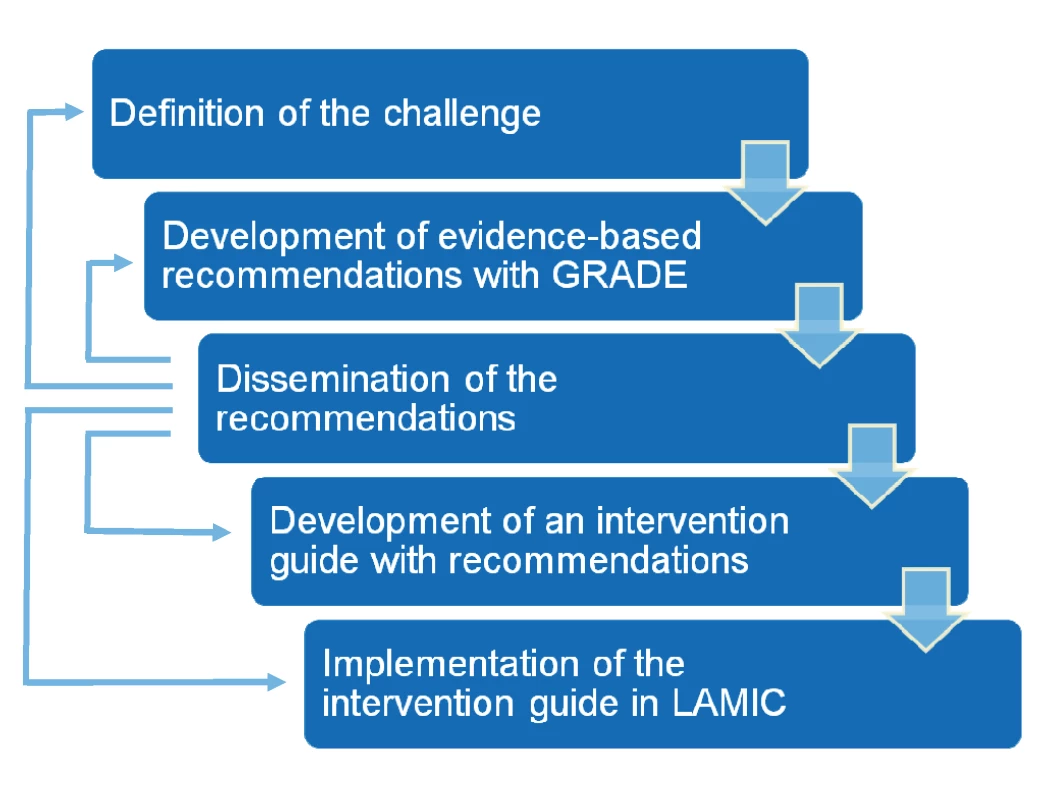
mhGAP Recommendations
WHO recommendations aim to be based on systematic reviews of the best available evidence and consideration of values, preferences, and feasibility issues from an international perspective and as reflected in relevant WHO policy documents and technical tools. Evidence profiles were developed for each of the priority conditions as well as a category labeled “other significant emotional or medically unexplained complaints.” Tables 1–8 provide the running title of the question and the abridged recommendations for each of the conditions. These recommendations focus on the management of MNS disorders in non-specialist settings in LAMIC. Each recommendation has a unique identifier—a short form of the priority condition and a number (e.g., DEP 1 for depression question 1). The detailed evidence profile can be accessed from the mhGAP Evidence Resource Centre (http://www.who.int/mental_health/mhgap/evidence/en/index.html).
Tab. 1. Abridged recommendations for depression (DEP 1–6) and other significant emotional or medically unexplained complaints (OTH 1–7). 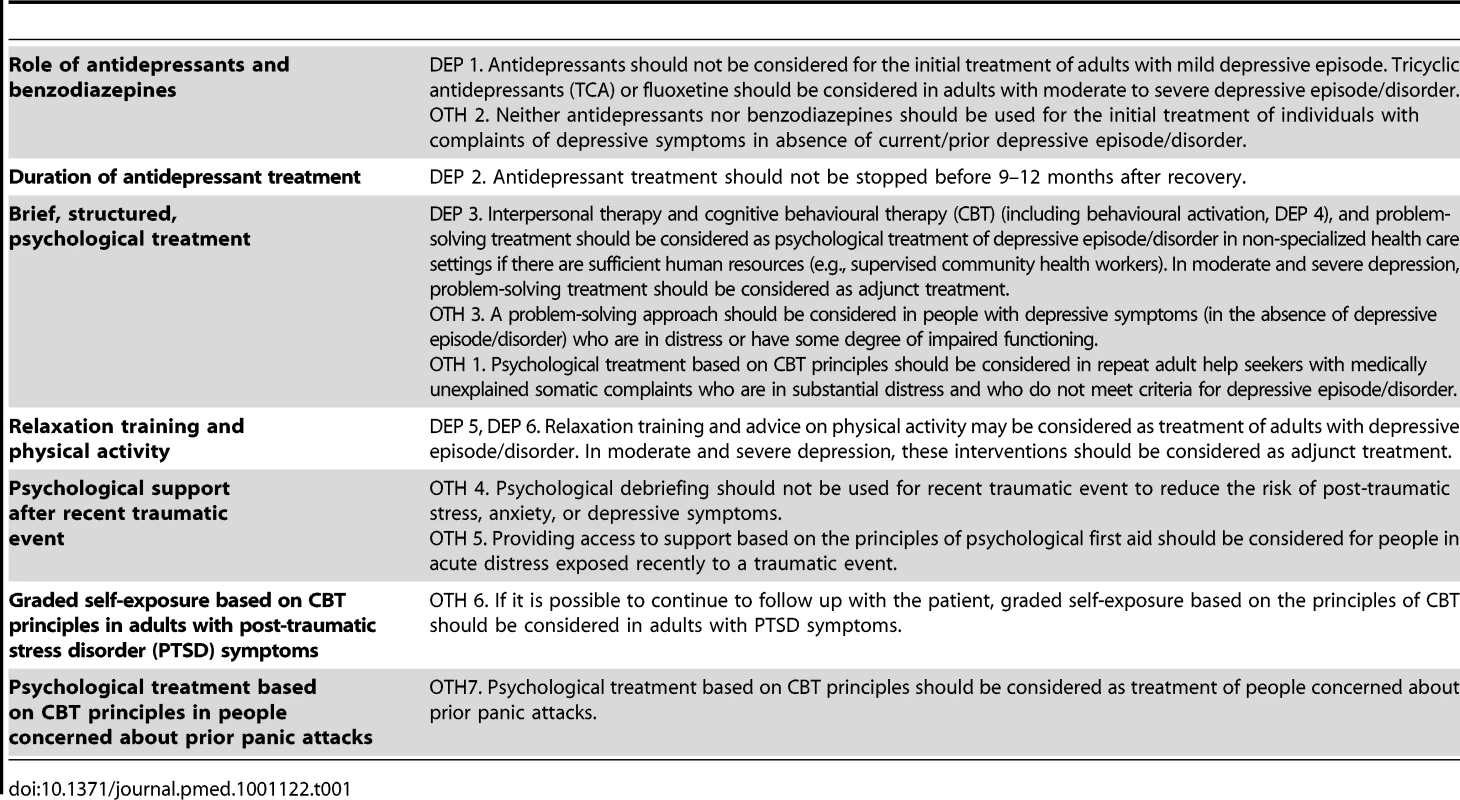
Tab. 2. Abridged recommendations for epilepsy and seizures (EPI 1–12). 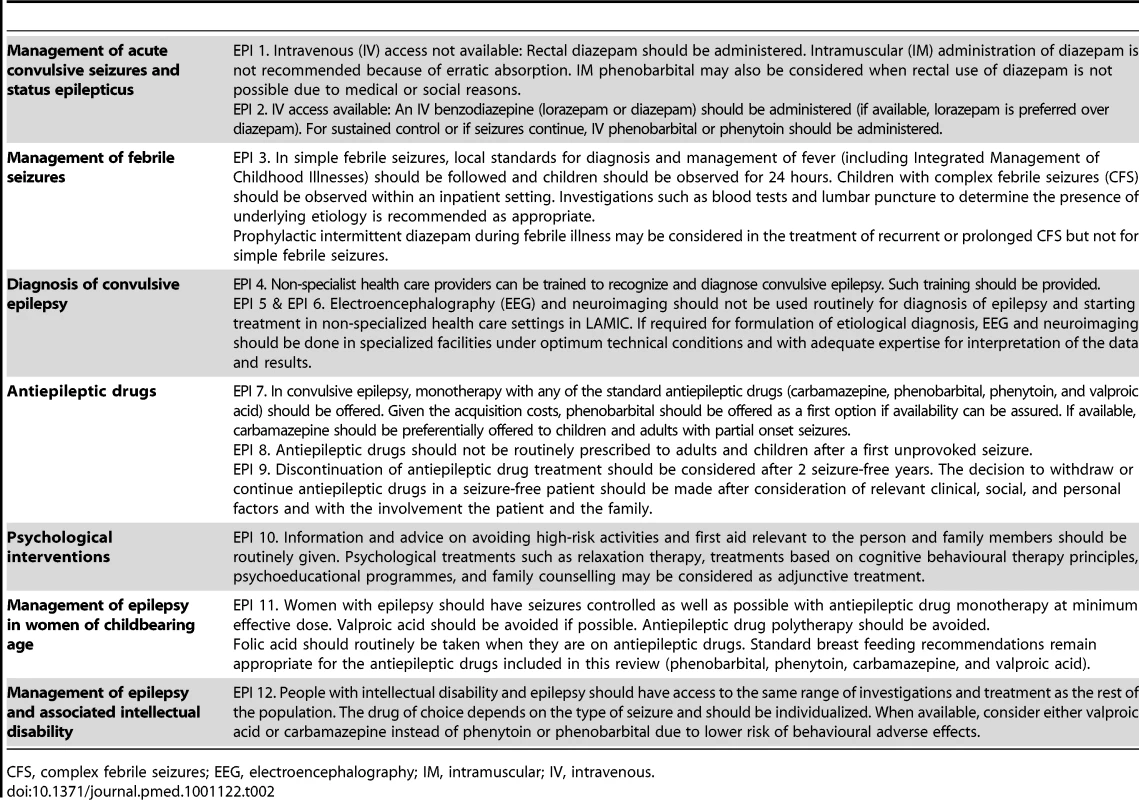
CFS, complex febrile seizures; EEG, electroencephalography; IM, intramuscular; IV, intravenous. Tab. 3. Abridged recommendations for psychosis and bipolar disorders (PSY 1–13). 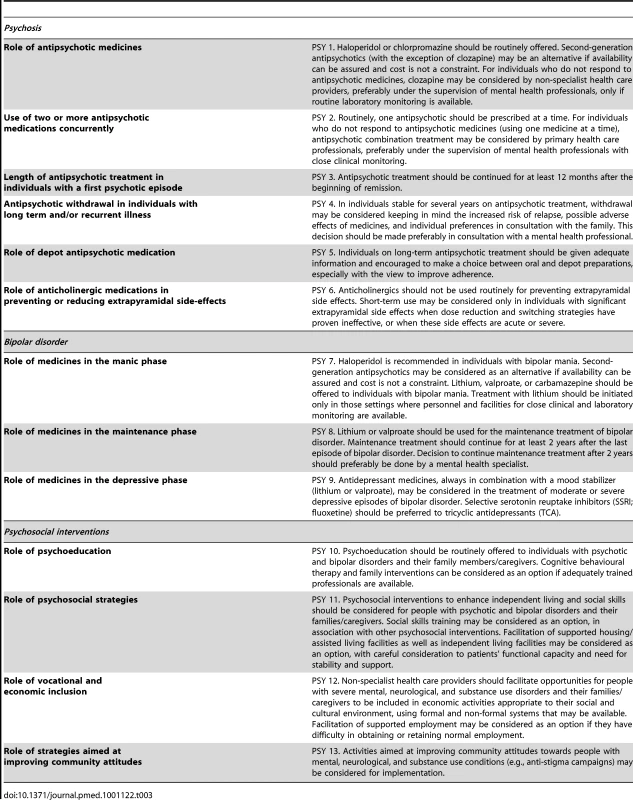
Tab. 4. Abridged recommendations for self-harm and suicide (SUI 1–9). 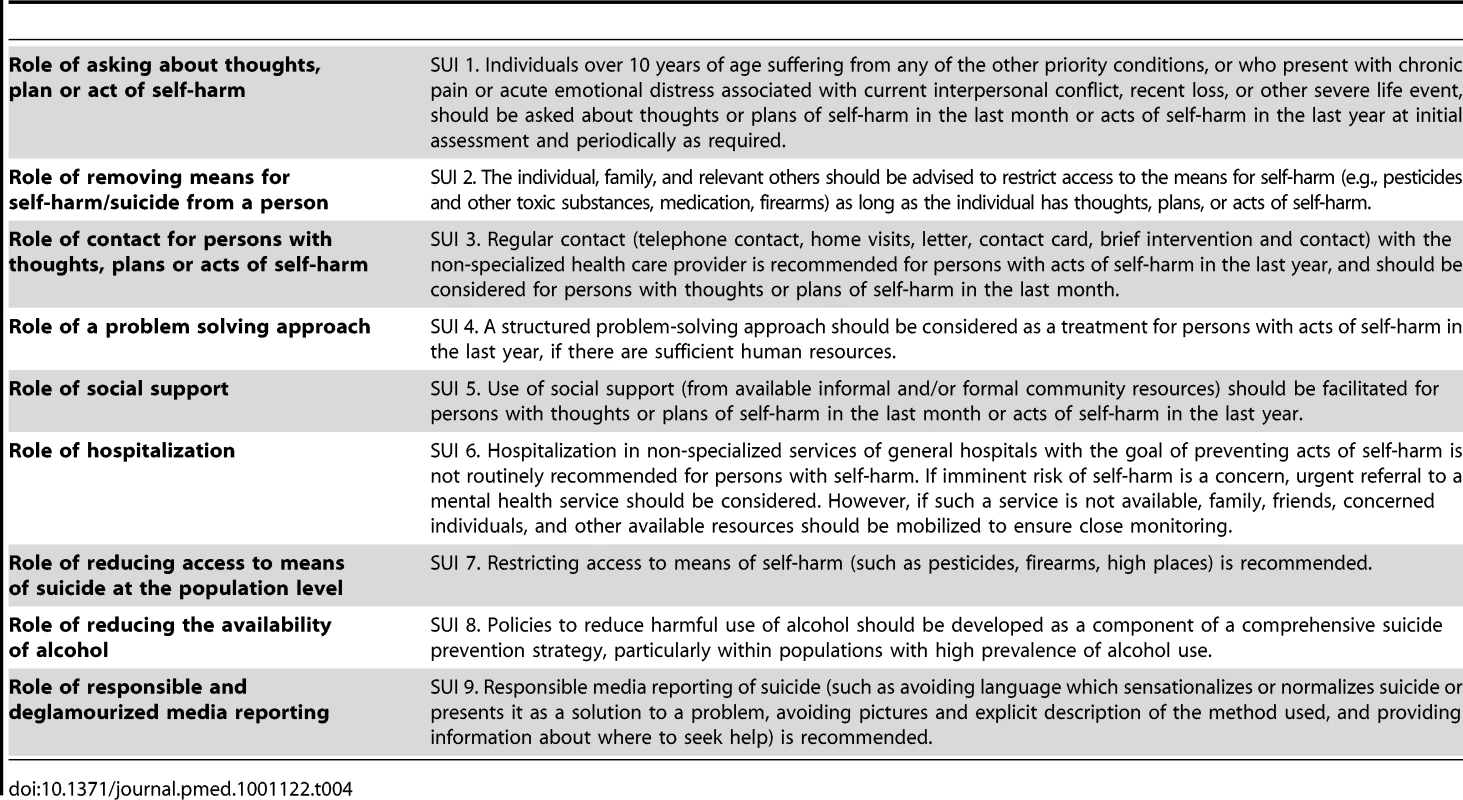
Tab. 5. Abridged recommendations for dementia (DEM 1–10). 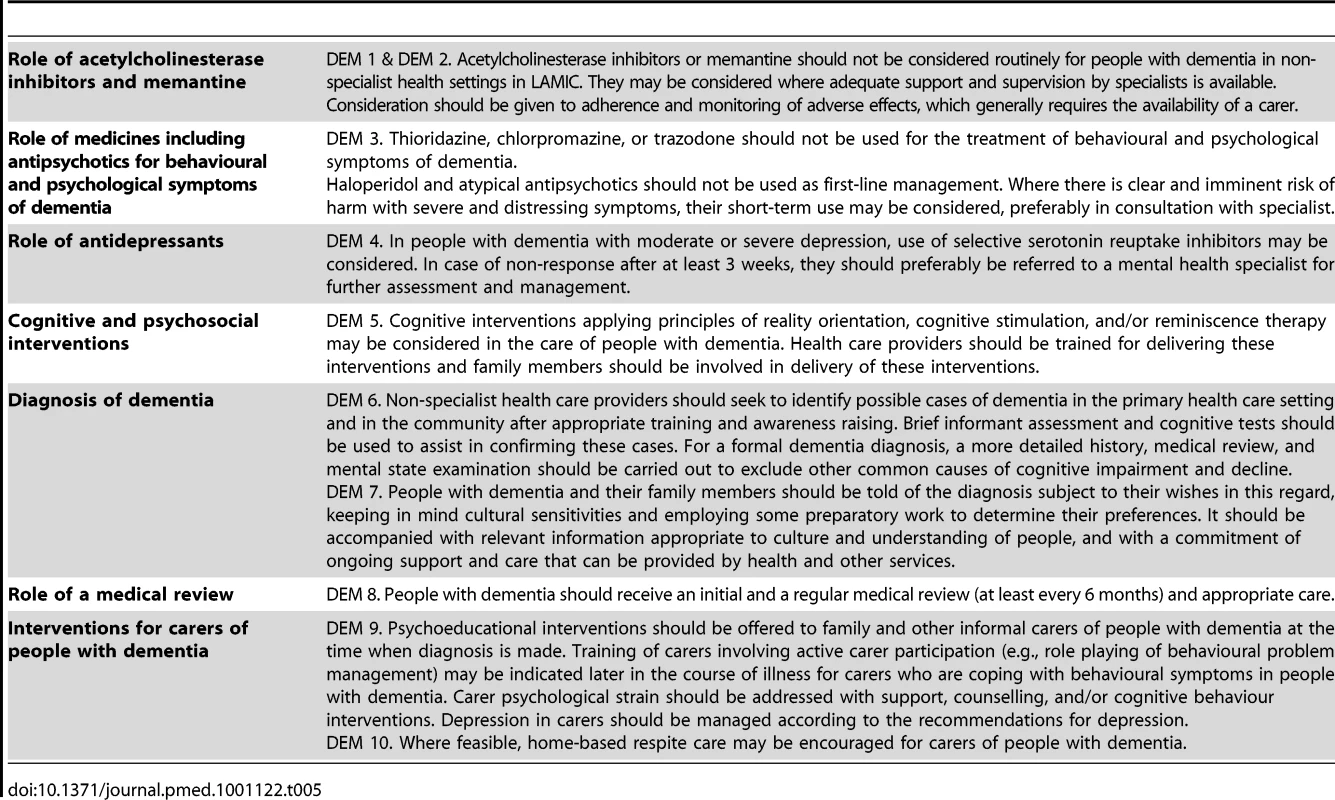
Tab. 6. Abridged recommendations for alcohol use disorders (ALC 1–6). 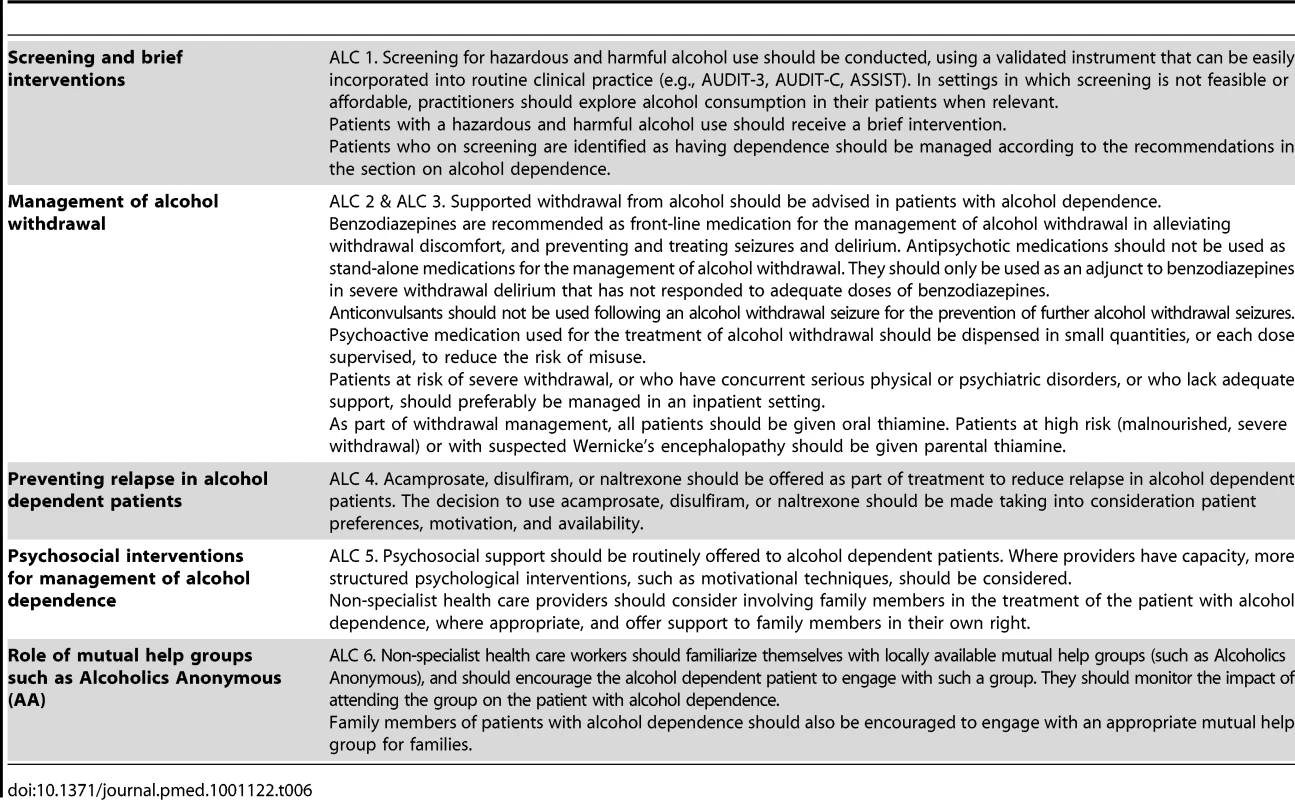
Tab. 7. Abridged recommendations for drug use disorders (DRU 1–6). 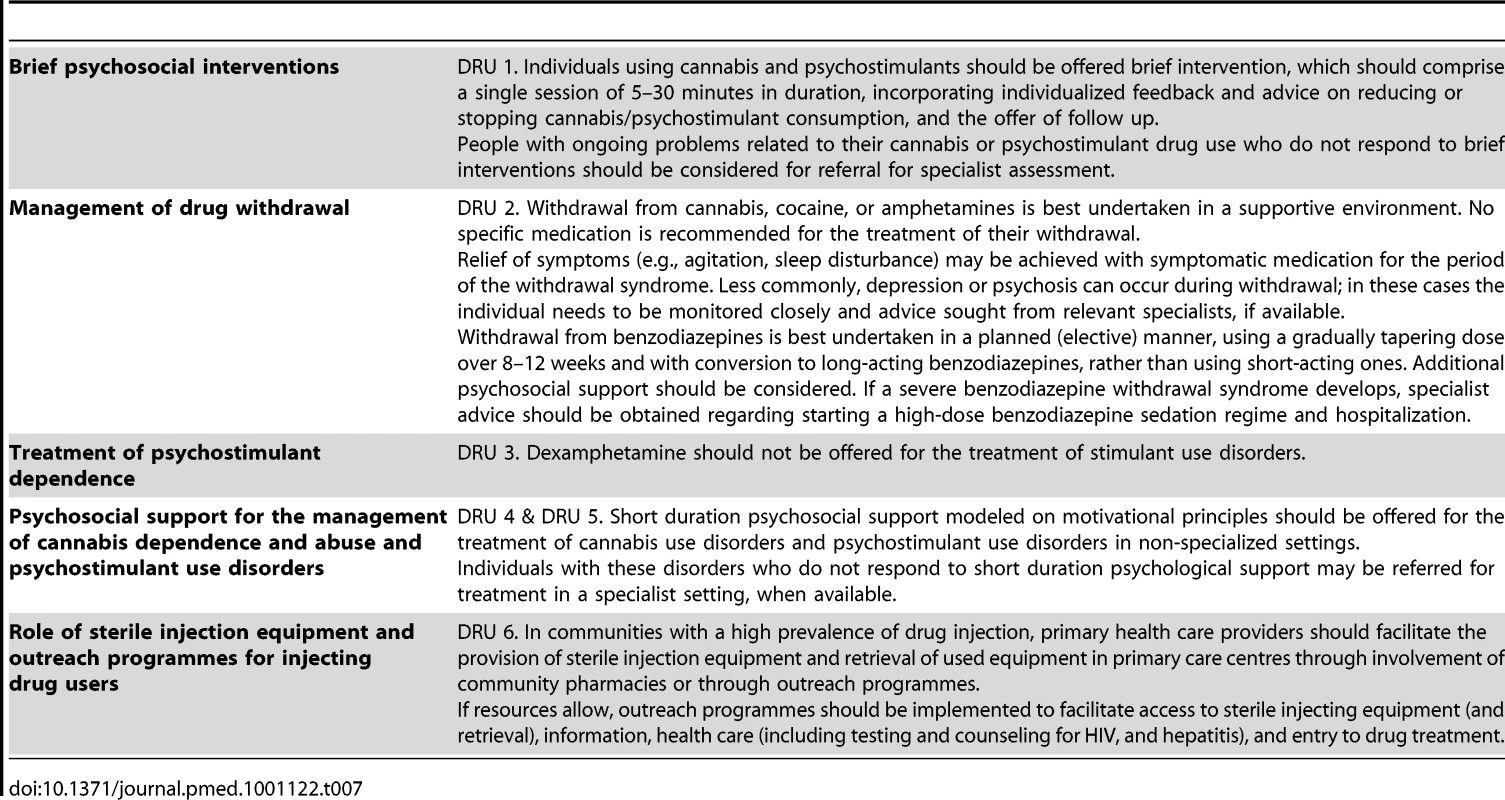
Tab. 8. Abridged recommendations for child and adolescent mental health conditions (CAMH 1–13). 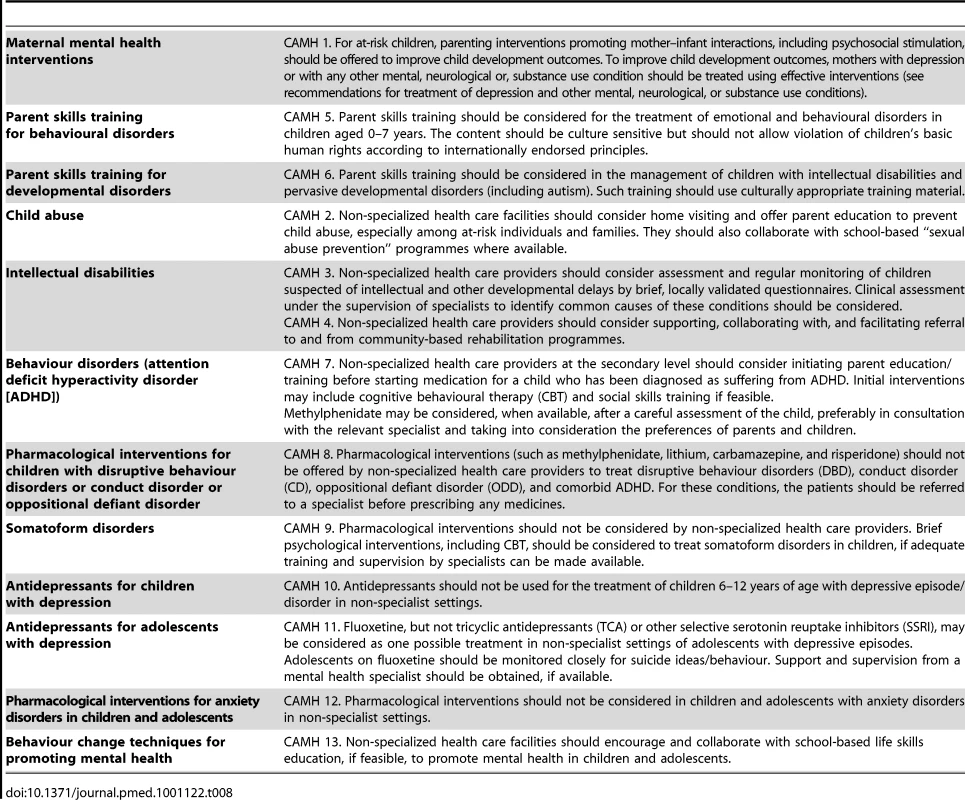
Strengths and Limitations of the Process
Developing recommendations is a complex process that involves systematic review and assessment of the quality of evidence and balance of benefits and harms. In addition, explicit consideration of other issues such as value judgments, resource use, and feasibility, which are major considerations, need to be incorporated. Developing mhGAP recommendations within this framework highlighted several challenging and critical issues, including difficulties in formulating questions and rating outcomes, potential reproducibility and consistency problems, problems in incorporating observational evidence when evidence in the form of randomized trials was not available, and difficulties in defining how values, preferences, and feasibility issues should be considered, as the methodology for these aspects is much less developed [12].
The mhGAP guidelines highlight issues where uncertainty or controversy exists or areas where a change in policy or clinical practice is needed. Table 9 provides examples of some areas where the review of evidence, values, and resource considerations supported the change required in clinical practice.
Tab. 9. Clinical practice implications of mhGAP recommendations. 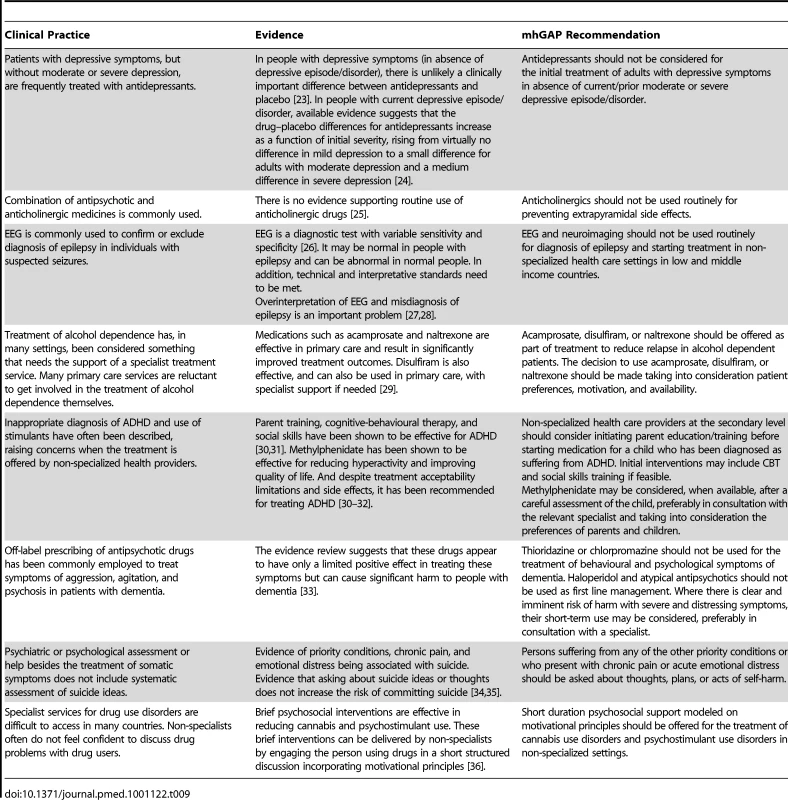
One of the most challenging aspects of the whole process was that while for some mental health areas the background evidence was quite robust, for others the conventional way of synthesizing and evaluating the evidence revealed no or very poor quality evidence that was insufficient to make any recommendation. For example, some psychosocial interventions for individuals with psychosis or bipolar disorder are backed by few studies that provide inconclusive results. In such instances we took advantage of the GRADE methodology, which clearly recognizes that in addition to the evidence base, other aspects that are expected to inform the recommendations include consideration of values such as protection of human rights, feasibility and resource use, and GDG professional experience and their tacit knowledge. As previously noted, the added value of GRADE in these circumstances is that it requires GDG to transparently report that some recommendations are based on strong values and weak evidence [12]. By contrast, in other areas where a substantial amount of evidence is available, positive recommendations could not be issued due to considerations on feasibility aspects. For example, full cognitive behavioural therapy may be hardly feasible in many low - and middle-income settings considering the training, supervision, and time needed for this intervention, and taking into consideration the need for local adaptations. Similarly, drug treatments that require regular blood checks may not be recommended in settings where no infrastructure is available to provide such checks on a continuous basis.
Another challenging aspect was that while the main focus of WHO's mental health work was to develop recommendations for health care providers in low - and middle-income settings, most of the evidence comes from specialist settings of high-income countries. Despite this, we developed and applied instructions to overcome this compelling issue [12]; increasing implementation research in the contexts where the guidelines should eventually be applied would seem the best approach to enhance the applicability of research findings into practice.
Maintaining and Updating mhGAP Recommendations
Maintaining and updating evidence-based recommendations is similarly relevant, as new evidence is continuously generated and accumulated in the international literature. Updating of mhGAP recommendations will not only be based on this new evidence, but also on feedback from health care professionals, policy-makers, scientists, and public health experts involved in implementing the guidelines. We also expect that revisions might include review of new questions or areas currently not covered by mhGAP guidelines, which might be identified as relevant questions to be addressed. In order to facilitate and encourage feedback, an electronically accessible web repository of recommendations and background material, including all the evidence profiles that were used to generate the recommendations, has recently been developed and will be regularly maintained and updated (http://www.who.int/mental_health/mhgap/evidence/en/index.html). The readers of this article can also provide their feedback by posting comments online at PLoS Medicine. WHO will follow a systematic procedure for updating the recommendations following the same strict and transparent methodological process that was employed for their initial development.
Guideline Implementation Issues
Scaling up delivery of interventions and achieving a desirable level of mental health care quality requires a dynamic and collaborative approach. Research findings that are generated by studies and trials should guide health care providers when making decisions in clinical practice. However, it is very difficult for the individual health care provider to interpret the existing evidence coming from randomized controlled trials, observational studies, and other sources of scientific evidence. Even if the evidence is systematically reviewed, the translation into the relevant policy and programme decisions, as well as the implementation in practice, is not straightforward. Effective strategies, techniques, and incentives are needed to disseminate and implement the guidelines. Finally, the interventions need to be adopted and integrated into practice by providers at all levels [13].
In the field of mental health care, the issue of how guidelines should be implemented to maximize their impact on clinician performance and patient outcome has rarely been investigated. A recent meta-analysis of different guideline implementation strategies included only 18 studies, nine of which were randomized trials [14]. The analysis of these 18 studies revealed that multifaceted interventions were more likely to have an impact on clinician performance and patient outcome, albeit effect sizes were generally modest. Additionally, it has been shown that audit of clinical activities and feedback to doctors may be a relevant component of any implementation strategy [15]. These findings are in line with those of a landmark systematic review of implementation studies [16].
The scarce evidence base on how guidelines should be implemented must not weaken international efforts to develop and evaluate implementation plans [17]. As part of the WHO implementation strategy, mhGAP recommendations have been incorporated into an integrated package of interventions called mhGAP Intervention Guide (mhGAP-IG) for Mental, Neurological and Substance Use Disorders in Non-specialized Health Settings [18]. The mhGAP-IG translates the evidence-based recommendations into simple clinical protocols and algorithms to facilitate decision making for assessment and management. It is aimed at non-specialist health care providers working at first - and second-level facilities. It is important that they are trained and then supervised and supported by the specialists.
The mhGAP-IG provides an integrated package of interventions for the management of priority MNS disorders. The reasons for integrated packages are the following: one, packages are an effective and efficient way of improving health service delivery. Two, delivery of interventions as a package is relatively cost-effective in terms of training and supervision. Many interventions and conditions go naturally together because they can be delivered by the same person at different times and because a limited range of interventions are applicable to a variety of conditions. Three, packages help concentrate scarce resources on the services that provide the best “value for the money”. We believe that the implementation of mhGAP guidelines and scaling them up would lead to a decrease in the burden of MNS disorders. For example, 7 million DALYs (11% of burden due to depression) are avertable with 50% coverage with interventions for depression (anti-depressant drugs [generic TCAs or SSRIs] plus brief psychotherapy) [19]. Similarly, 23% of burden due to epilepsy is avertable at 50% coverage with standard antiepileptic drugs [20]. Thus, the gains that are possible from scaling up of the integrated package could be substantial.
Although the mhGAP-IG is the principal clinical tool being used as part of the scaling up strategy of the mhGAP program in countries, accompanying training materials are being developed for capacity building. Program implementation using the mhGAP-IG has already started in four countries: Ethiopia, Jordan, Nigeria, and Panama [21]. There are a number of major implementation research questions that now need addressing. mhGAP has provided a definitive platform to define “what” should be scaled up. The “how” question needs answering now. An example of such an initiative is the multi-partner PRogramme for Improving Mental health carE (PRIME) Project, which has the objective to generate evidence on the implementation and scaling up of treatment programmes for priority mental disorders in low-resource settings [22]. In the near future, further efforts should be made to introduce formal evaluations of the capability of these programs to induce relevant and persistent changes, and to generate useful insights on how implementation in LAMIC should be conducted to maximize benefit at sustainable costs.
Box 1. Key mhGAP Implementation Research Areas
Although research in the field of mental, neurological, and substance use disorders has significantly advanced in recent years, most of these advancements have been driven by the needs of health systems in the richest countries. To appropriately translate research findings into clinical and public health practices, it is critical to accelerate implementation research to evaluate interventions beyond the controlled conditions of research settings, and in the type of populations that suffer the largest proportion of the global burden of morbidity and mortality.
Research areas that will help in scaling up mhGAP coverage include:
-
Strengthening human resources, including capacity development and task shifting issues
-
Improving health financing to avoid out-of-pocket and point-of-care payments for health care
-
Simplifying interventions so that they can be delivered with fewer resources
-
Identifying intervention delivery channels for greater reach and equity, and lower costs, including engagement of the non-government sector
-
Improving programme management and synergies between mental health and other programmes such as maternal or child health to overcome barriers to effective programme implementation
-
Mobilizing community resources for improved intervention delivery and increased health care utilization
Some examples of research questions are:
-
How can mental health care using mhGAP be “added upon” the existing maternal health programmes?
-
What are the specific barriers that hinder access to effective mental health interventions in rural populations?
-
How can we use electronic and mobile technology to improve follow up for people with mental, neurological, and substance use disorders?
-
How can the coverage, quality, and impact of mhGAP interventions improved by involving community health workers?
-
What is the cost to the health system of scaling up mhGAP interventions when delivered through routine primary health care?
Zdroje
1. World Health Organization 2008 Scaling up care for mental, neurological, and substance use disorders. Available: http://www.who.int/mental_health/mhgap_final_english.pdf. Accessed 10 October 2011
2. PrinceMPatelVSaxenaSMajMMaselkoJ 2007 No health without mental health. Lancet 370 859 877
3. SaxenaSThornicroftGKnappMWhitefordH 2007 Resources for mental health: scarcity, inequity and inefficiency. Lancet 370 878 889
4. PatelVArayaRChatterjeeSChisholmDCohenA 2007 Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet 370 991 1005
5. JacobKSSharanPMirzaIGarrido-CumbreraMSeedatS 2007 Mental health systems in countries: where are we now? Lancet 370 1061 1077
6. SaracenoBvan OmmerenMBatnijiRCohenAGurejeO 2007 Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 370 1164 1174
7. ChisholmDFlisherAJLundCPatelVSaxenaS 2007 Scale up services for mental disorders: a call for action. Lancet 370 1241 1252
8. World Health Organization 2008 The global burden of disease: 2004 update. Available: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf. Accessed 10 October 2011
9. World Health Organization 2010 Packages of interventions for family planning, safe abortion care, maternal, newborn and child health. Available: http://whqlibdoc.who.int/hq/2010/WHO_FCH_10.06_eng.pdf. Accessed 10 October 2011
10. CollinsPYPatelVJoestlSSMarchDInselTR 2011 Grand challenges in global mental health. Nature 475 27 30
11. PatelVThornicroftG 2009 Packages of care for mental, neurological, and substance use disorders in low - and middle-income countries. PLoS Med 6 e1000160 doi:10.1371/journal.pmed.1000160
12. BarbuiCDuaTvan OmmerenMYasamyMTFleischmannA 2010 Challenges in developing evidence-based recommendations using the GRADE approach: the case of mental, neurological, and substance use disorders. PLoS Med 7 e1000322 doi:10.1371/journal.pmed.1000322
13. BloomrosenMDetmerDE 2010 Informatics, evidence-based care, and research; implications for national policy: a report of an American Medical Informatics Association health policy conference. J Am Med Inform Assoc 17 115 123
14. WeinmannSKoestersMBeckerT 2007 Effects of implementation of psychiatric guidelines on provider performance and patient outcome: systematic review. Acta Psychiatr Scand 115 420 433
15. KnaupCKoestersMSchoeferDBeckerTPuschnerB 2009 Effect of feedback of treatment outcome in specialist mental healthcare: meta-analysis. Br J Psychiatry 195 15 22
16. GrimshawJMThomasREMacLennanGFraserCRamsayCR 2004 Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 8 iii iv, 1–72
17. TansellaMThornicroftG 2009 Implementation science: understanding the translation of evidence into practice. Br J Psychiatry 195 283 285
18. World Health Organization 2010 mhGAP intervention guide for for mental, neurological, and substance use disorders in non-specialized settings. Available: http://www.who.int/mental_health/evidence/mhGAP_intervention_guide/en/index.html. Accessed 10 October 2011
19. ChisholmDSandersonKAyuso-MateosJLSaxenaS 2004 Reducing the global burden of depression: population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry 184 393 403
20. ChisholmD WHO-CHOICE 2005 Cost-effectiveness of first-line antiepileptic drug treatments in the developing world: a population-level analysis. Epilepsia 46 751 759
21. WHO 2011 mhGAP newsletter. June 2011. Available: http://www.who.int/mental_health/mhGAP_nl__jun2011_en.pdf. Accessed 15 October 2011
22. University of Cape Town 11 February 2011 New project to PRIME mental health services. Available: http://www.uct.ac.za/print/dailynews/?id=7691. Accessed 10 October 2011
23. BarbuiCCiprianiAPatelVAyuso-MateosJLvan OmmerenM 2011 Efficacy of antidepressants and benzodiazepines in minor depression: systematic review and meta-analysis. Br J Psychiatry 198 11 16, sup 1
24. KirschIDeaconBJHuedo-MedinaTBScoboriaAMooreTJ 2008 Initial severity and antidepressant benefits: a metaanalysis of data submitted to the Food and Drug Administration. PLoS Med 5 e45 doi:10.1371/journal.pmed.0050045
25. RathboneJSoares-WeiserK 2006 Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev 4 CD003727
26. FowleAJBinnieCD 2000 Uses and abuses of the EEG in epilepsy. Epilepsia 41 Suppl 3 S10 S18
27. EngelJJr 1984 A practical guide for routine EEG studies in epilepsy. J Clin Neurophysiol 1 109 142
28. BenbadisSRTatumWO 2003 Overintepretation of EEGs and misdiagnosis of epilepsy. J Clin Neurophysiol 20 42 44
29. RosnerSLeuchtSLehertPSoykaetM 2008 Acamprosate supports abstinence, naltrexone prevents excessive drinking: evidence from a meta-analysis with unreported outcomes. Psychopharmacology 22 11 23
30. GhumanJKArnoldLEAnthonyBJ 2008 Psychopharmacological and other treatments in preschool children with attention-deficit/hyperactivity disorder: current evidence and practice. J Child Adolesc Psychopharmacol 18 413 447
31. NICE 2009 Attention deficit hyperactivity disorder. The NICE guideline on diagnosis and management of ADHD in children, young people and adults. Section 7.2.14. From evidence to recommendations: psychological interventions for children and young people with ADHD. NICE technology appraisal 72 London National Institute for Health and Clinical Excellence
32. KingSGriffinSHodgesZWeatherlyHAsseburgC 2006 A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents. Health Technol Assess 10 1 162
33. BanerjeeS 2009 The use of antipsychotic medication for people with dementia: time for action. A report for the Minister of State for Care Services. London: Department of Health. Available: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_108302.pdf. Accessed 10 October 2011
34. BeautraisALJoycePRMulderRTFergussonDMDeavollBJ 1996 Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry 153 1009 1014
35. LejoyeuxMHuetFClaudonMFichelleACasalinoE 2008 Characteristics of suicide attempts preceded by alcohol consumption. Arch Suicide Res 12 30 38
36. DenisCLavieEFatseasMAuriacombeM 2006 Psychotherapeutic interventions for cannabis abuse and/or dependence in outpatient settings. Cochrane Database of Systematic Reviews 3 CD005336
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2011 Číslo 11- Léčba bolesti u seniorů
- Benefity fixní kombinace tramadolu a paracetamolu v léčbě bolesti
- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Flexofytol® – přírodní revoluce v boji proti osteoartróze kloubů
- Superoxidované roztoky v prevenci infekcí u dialyzovaných pacientů
-
Všechny články tohoto čísla
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Voluntary Medical Male Circumcision: Translating Research into the Rapid Expansion of Services in Kenya, 2008–2011
- Quality of Maternal Health Care: A Call for Papers for a Maternal Health Task Force–PLoS Collection
- Voluntary Medical Male Circumcision: Matching Demand and Supply with Quality and Efficiency in a High-Volume Campaign in Iringa Region, Tanzania
- Priorities for Research on Equity and Health: Towards an Equity-Focused Health Research Agenda
- What Research Is Needed to Stop TB? Introducing the
- Responsible Governance for Mental Health Research in Low Resource Countries
- Voluntary Medical Male Circumcision: Modeling the Impact and Cost of Expanding Male Circumcision for HIV Prevention in Eastern and Southern Africa
- Effect of Supplementation with Zinc and Other Micronutrients on Malaria in Tanzanian Children: A Randomised Trial
- HIV, Gender, Race, Sexual Orientation, and Sex Work: A Qualitative Study of Intersectional Stigma Experienced by HIV-Positive Women in Ontario, Canada
- Voluntary Medical Male Circumcision: A Framework Analysis of Policy and Program Implementation in Eastern and Southern Africa
- Voluntary Medical Male Circumcision: Logistics, Commodities, and Waste Management Requirements for Scale-Up of Services
- Optimal Uses of Antiretrovirals for Prevention in HIV-1 Serodiscordant Heterosexual Couples in South Africa: A Modelling Study
- Managing the Demand for Global Health Education
- Post-neonatal Mortality, Morbidity, and Developmental Outcome after Ultrasound-Dated Preterm Birth in Rural Malawi: A Community-Based Cohort Study
- Voluntary Medical Male Circumcision: An Introduction to the Cost, Impact, and Challenges of Accelerated Scaling Up
- On the Futility of Screening for Genes That Make You Fat
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
- A Head-to-Head Comparison of Four Artemisinin-Based Combinations for Treating Uncomplicated Malaria in African Children: A Randomized Trial
- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Evidence-Based Guidelines for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: Summary of WHO Recommendations
- Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa
- Rapid Diagnosis of Tuberculosis with the Xpert MTB/RIF Assay in High Burden Countries: A Cost-Effectiveness Analysis
- Physical Activity Attenuates the Influence of Variants on Obesity Risk: A Meta-Analysis of 218,166 Adults and 19,268 Children
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



