-
Články
Reklama
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
ReklamaGene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
Background:
Colon cancer (CC) pathological staging fails to accurately predict recurrence, and to date, no gene expression signature has proven reliable for prognosis stratification in clinical practice, perhaps because CC is a heterogeneous disease. The aim of this study was to establish a comprehensive molecular classification of CC based on mRNA expression profile analyses.Methods and Findings:
Fresh-frozen primary tumor samples from a large multicenter cohort of 750 patients with stage I to IV CC who underwent surgery between 1987 and 2007 in seven centers were characterized for common DNA alterations, including BRAF, KRAS, and TP53 mutations, CpG island methylator phenotype, mismatch repair status, and chromosomal instability status, and were screened with whole genome and transcriptome arrays. 566 samples fulfilled RNA quality requirements. Unsupervised consensus hierarchical clustering applied to gene expression data from a discovery subset of 443 CC samples identified six molecular subtypes. These subtypes were associated with distinct clinicopathological characteristics, molecular alterations, specific enrichments of supervised gene expression signatures (stem cell phenotype–like, normal-like, serrated CC phenotype–like), and deregulated signaling pathways. Based on their main biological characteristics, we distinguished a deficient mismatch repair subtype, a KRAS mutant subtype, a cancer stem cell subtype, and three chromosomal instability subtypes, including one associated with down-regulated immune pathways, one with up-regulation of the Wnt pathway, and one displaying a normal-like gene expression profile. The classification was validated in the remaining 123 samples plus an independent set of 1,058 CC samples, including eight public datasets. Furthermore, prognosis was analyzed in the subset of stage II–III CC samples. The subtypes C4 and C6, but not the subtypes C1, C2, C3, and C5, were independently associated with shorter relapse-free survival, even after adjusting for age, sex, stage, and the emerging prognostic classifier Oncotype DX Colon Cancer Assay recurrence score (hazard ratio 1.5, 95% CI 1.1–2.1, p = 0.0097). However, a limitation of this study is that information on tumor grade and number of nodes examined was not available.Conclusions:
We describe the first, to our knowledge, robust transcriptome-based classification of CC that improves the current disease stratification based on clinicopathological variables and common DNA markers. The biological relevance of these subtypes is illustrated by significant differences in prognosis. This analysis provides possibilities for improving prognostic models and therapeutic strategies. In conclusion, we report a new classification of CC into six molecular subtypes that arise through distinct biological pathways.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(5): e32767. doi:10.1371/journal.pmed.1001453
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001453Summary
Background:
Colon cancer (CC) pathological staging fails to accurately predict recurrence, and to date, no gene expression signature has proven reliable for prognosis stratification in clinical practice, perhaps because CC is a heterogeneous disease. The aim of this study was to establish a comprehensive molecular classification of CC based on mRNA expression profile analyses.Methods and Findings:
Fresh-frozen primary tumor samples from a large multicenter cohort of 750 patients with stage I to IV CC who underwent surgery between 1987 and 2007 in seven centers were characterized for common DNA alterations, including BRAF, KRAS, and TP53 mutations, CpG island methylator phenotype, mismatch repair status, and chromosomal instability status, and were screened with whole genome and transcriptome arrays. 566 samples fulfilled RNA quality requirements. Unsupervised consensus hierarchical clustering applied to gene expression data from a discovery subset of 443 CC samples identified six molecular subtypes. These subtypes were associated with distinct clinicopathological characteristics, molecular alterations, specific enrichments of supervised gene expression signatures (stem cell phenotype–like, normal-like, serrated CC phenotype–like), and deregulated signaling pathways. Based on their main biological characteristics, we distinguished a deficient mismatch repair subtype, a KRAS mutant subtype, a cancer stem cell subtype, and three chromosomal instability subtypes, including one associated with down-regulated immune pathways, one with up-regulation of the Wnt pathway, and one displaying a normal-like gene expression profile. The classification was validated in the remaining 123 samples plus an independent set of 1,058 CC samples, including eight public datasets. Furthermore, prognosis was analyzed in the subset of stage II–III CC samples. The subtypes C4 and C6, but not the subtypes C1, C2, C3, and C5, were independently associated with shorter relapse-free survival, even after adjusting for age, sex, stage, and the emerging prognostic classifier Oncotype DX Colon Cancer Assay recurrence score (hazard ratio 1.5, 95% CI 1.1–2.1, p = 0.0097). However, a limitation of this study is that information on tumor grade and number of nodes examined was not available.Conclusions:
We describe the first, to our knowledge, robust transcriptome-based classification of CC that improves the current disease stratification based on clinicopathological variables and common DNA markers. The biological relevance of these subtypes is illustrated by significant differences in prognosis. This analysis provides possibilities for improving prognostic models and therapeutic strategies. In conclusion, we report a new classification of CC into six molecular subtypes that arise through distinct biological pathways.
Please see later in the article for the Editors' SummaryIntroduction
Despite advances in screening, diagnosis, and treatment, colorectal cancer (CRC) is the third most common cancer and the fourth-leading cause of cancer death worldwide [1]. Pathological staging is the only prognostic classification used in clinical practice to select patients for adjuvant chemotherapy [2]. However, pathological staging fails to predict recurrence accurately in many patients undergoing curative surgery for localized CRC. In fact, 10%–20% of patients with stage II CRC, and 30%–40% of those with stage III CRC, develop recurrence. Among the molecular markers that have been extensively investigated for colon cancer (CC) characterization and prognosis, microsatellite instability (MSI), caused by defective function of the DNA mismatch repair (MMR) system, is the only marker that was reproducibly found to be a significant prognostic factor in early CRC in both a meta-analysis and a prospective trial [3],[4]. Many studies have exploited microarray technology to investigate gene expression profiles (GEPs) in CRC in recent years, but no established signature has been found that is useful for clinical practice, especially for predicting prognosis [5]–[8]. GEP studies on CRC have been only poorly reproducible, possibly because CRC is composed of distinct molecular entities that may develop through multiple pathways on the basis of different molecular features [9]–[11]. As a consequence, there may be several prognostic signatures for CRC, each corresponding to a different entity. Indeed, GEP studies that include unsupervised hierarchical clustering, and integrated genetic/epigenetic analysis—including the more recent classification based on high-throughput methylome data [12]—have identified at least three distinct molecular subtypes of CC [7],[9]–[13]. Therefore, CC should no longer be considered as a homogeneous entity. However, the molecular classification of CC currently used, which is based on a few common DNA markers (MSI, CpG island methylator phenotype [CIMP], chromosomal instability [CIN], and BRAF and KRAS mutations) [9]–[11], needs to be refined, and a standard and reproducible molecular classification is still not available.
In this study, we exploited a large, multicenter, and extensively characterized series of CC samples to establish a robust molecular classification based on genome-wide mRNA expression analysis. Then we assessed the associations between molecular subtypes and clinicopathological factors, common DNA alterations, and prognosis. To confirm the robustness of the subtypes obtained, we further validated our molecular classification in a large independent set.
Methods
Ethics Committee Approval
The use of the tumor collection was approved by the following ethics committees and institutional boards: lle de France II (2008-135; AFSSAP 2008-A01058-47), Marseille (PHRC2005, COS-IPC of 27 September 2007), Strasbourg (Comité Consultatif de Protection des Personnes dans la Recherche Biomedicale d'Alsace, 2004-63 and CPP-EST4 [DC-2009-1016 and AC-2008-438]), the Human Research Ethics Committee of Saint-Antoine Hospital (INCa; TUM0203—project 2010-1-RT-02), the Toulouse Hospital board (CRB–Cancer Toulouse, DC-2008-463, AC-2008-820, CPP2), and Nice (PHRC1997, CHUNice-948). The informed consent of the patients was recorded as required by a French law in force until 2007. Since the last inclusion in this study was 2007, the standard hospital blanket consent was considered sufficient.
Patients
The French national Cartes d'Identité des Tumeurs (CIT) program involves a multicenter cohort of 750 patients with stage I to IV CC who underwent surgery between 1987 and 2007 in seven centers. Fresh-frozen primary tumor tissue samples were retrospectively collected at the Institut Gustave Roussy (Villejuif), the Hôpital Saint Antoine (Paris), the Hôpital Européen Georges Pompidou (Paris), the Hôpital de Hautepierre (Strasbourg), the Hôpital Purpan (Toulouse), and the Institut Paoli-Calmettes (Marseille), and prospectively collected at the Centre Antoine Lacassagne (Nice). Patients who received preoperative chemotherapy and/or radiation therapy and those with primary rectal cancer were excluded from this study. Clinical and pathologic data were extracted from the medical records and centrally reviewed for the purpose of this study. Patients were staged according to the American Joint Committee on Cancer tumor node metastasis (TNM) staging system [2] and monitored for relapse (distant and/or locoregional recurrence; median follow-up of 51.5 mo). Patient and tumor characteristics are summarized in Table 1 and detailed in Table S1.
Tab. 1. Patient and tumor characteristics of the different sets. 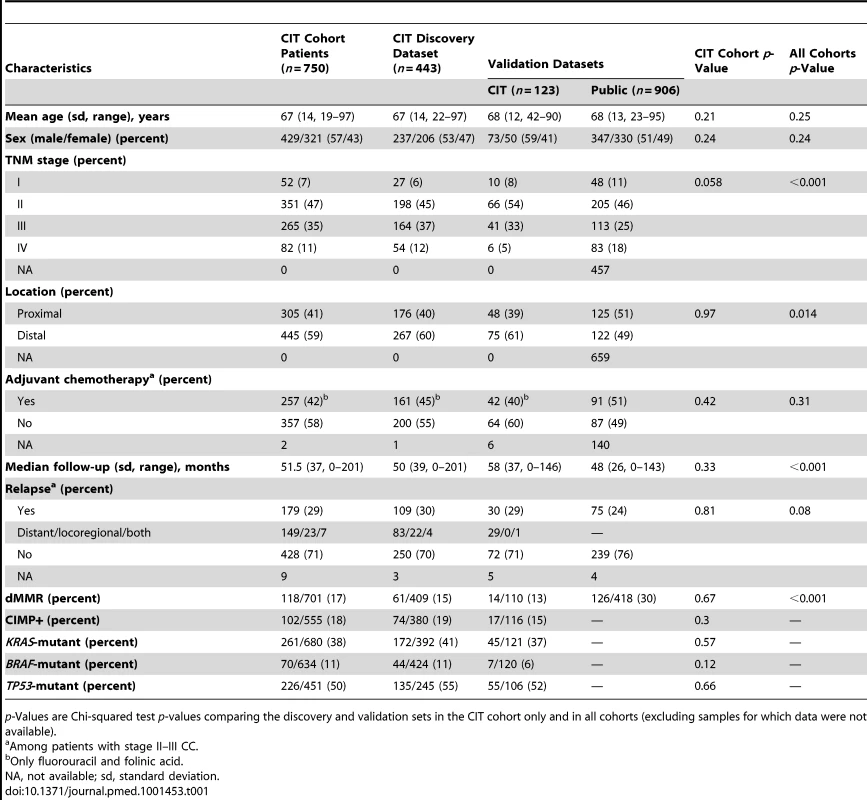
p-Values are Chi-squared test p-values comparing the discovery and validation sets in the CIT cohort only and in all cohorts (excluding samples for which data were not available). Of the 750 tumor samples of the CIT cohort, 566 fulfilled RNA quality requirements for GEP analysis (Figure S1). The 566 samples were split into a discovery set (n = 443) and a validation set (n = 123), well balanced for the main anatomoclinical characteristics (Table 1). The validation set also included 906 CC samples available from seven public datasets (GSE13067, GSE13294, GSE14333, GSE17536/17537, GSE18088, GSE26682, and GSE33113). These datasets corresponded to all available public datasets fulfilling the following criteria: available GEP data obtained using a similar chip platform (Affymetrix U133 Plus 2.0 chips) with raw data CEL files, and tumor location and either common DNA alteration (n = 457) and/or patient outcome (n = 449) data available. Within the discovery (n = 443) and the validation (n = 1,029) sets, 359 and 416 patients with stage II–III CC and documented relapse-free survival (RFS) were available for survival analysis, respectively (Figure S1). The dataset from The Cancer Genome Atlas (TCGA) [13], although obtained using a non-Affymetrix platform and therefore analyzed separately, was added to the validation set because of the extensive DNA alteration annotations provided for 152 CC samples.
Gene Mutations, MMR Status, and CIMP Analysis
The seven most frequent mutations in codons 12 and 13 of KRAS were assessed as previously described [14]. The BRAF c.1799T>A (p.V600E) mutation was assessed by allelic discrimination using TaqMan probes and the same protocol as that for KRAS mutations. TP53 mutations (exons 4–9) were assessed as previously described [15]. MSI was analyzed using a panel of five different microsatellite loci from the Bethesda reference panel [16]. MSI-high tumors were further classified as deficient MMR (dMMR), and both MSI-low and MSS tumors as proficient MMR (pMMR). CIMP status was determined using a panel of five markers (CACNA1G, IGF2, NEUROG1, RUNX3, and SOCS1) as previously described [17]. Experimental procedures are detailed in Text S1. Common DNA alterations are summarized in Table 1 and detailed in Table S1.
Gene Expression Analysis
The GEP of 566 primary CC samples were determined on Affymetrix U133 Plus 2.0 chips. For 19 patients, adjacent non-tumor tissue (normal tissue [NT]) was also available and was tested. The methods used for RNA purification, quality control, fluorescent probe production, hybridization, and raw data processing were as previously described [18]. Each dataset was normalized independently in batches using the robust multi-array average method implemented in the R package affy [19]. For the CIT dataset, residual technical batch effects were corrected using the ComBat method implemented in the SVA R package [20]. Data are available via the NCBI Gene Expression Omnibus (http://www.ncbi.nlm.nih.gov/geo/; accession number GSE39582).
Array-Based Comparative Genomic Hybridization Analysis
A total of 464 of the 750 primary CC samples from the CIT cohort could be analyzed for array-based comparative genomic hybridization (CGH) on a BAC array containing 4,434 bacterial artificial chromosome clones with a median resolution of 0.6 Mb. DNA labeling, hybridization, and data processing were as previously described [21]. CIN was defined from CGH profiles: samples with at least 20% gain or loss of whole chromosomes or fractions of chromosomes were scored as CIN+ (see Text S1 for details).
Unsupervised Subtype Discovery Based on Gene Expression Analysis
Unsupervised classification of the discovery set was performed using hierarchical clustering (Ward linkage and 1 − Pearson correlation coefficient distance used) on the most variant class of probe sets (n = 1,459). To obtain a robust classification, we used a consensus unsupervised approach [22] implemented in the R package ConsensusClusterPlus. The consensus clusters were obtained from 1,000 resampling iterations of the hierarchical clustering, by randomly selecting a fraction of the samples and of the most variant probe sets (90%). The optimal number of clusters was selected according to the approach criteria detailed in Text S1.
Validation Set Subtype Assignment
Validation datasets were independently assigned to GEP subtypes according to a standard distance-to-centroid approach [23]. A centroid-based predictor was built by a 10-fold cross-validation approach, resulting in the selection of the five top up-regulated and five top down-regulated genes specific to each subtype, yielding 57 genes (three genes were shared by two subtypes). The approach was implemented in the R package citccmst, and is detailed in Text S1.
Molecular Subtype Characterization
The Chi-squared test and logistic regression were used to study associations between anatomoclinical features, common DNA alterations, and subtypes. Each molecular subtype was further characterized according to (i) GEP of NT counterparts from our dataset; (ii) previously published supervised signatures based on intestinal stem cell phenotype [24],[25], BRAF mutation [26], and serrated CRC phenotype [27], as described in Text S1; (iii) cancer-relevant signaling pathways retrieved from the Kyoto Encyclopedia of Genes and Genomes (see Text S1); and (iv) CGH alteration frequencies.
Recurrence Risk Group Assignment according to Other Molecular Predictors
The ColoPrint and Oncotype DX prognostic classifiers [7],[8] were adapted and applied to our overall datasets as described in Text S1.
Survival Analysis
Survival analysis was intentionally restricted to the subgroup of patients with stage II–III tumors because reliable prognostic biomarkers are most needed for these patients. Indeed, most stage I patients will not derive benefit from adjuvant chemotherapy because of their excellent prognosis after curative surgery, and most stage IV patients, already metastatic, will die from their disease and therefore should be analyzed independently for progression-free survival. RFS was defined as the time from surgery to the first recurrence and was censored at 5 y. Survival was analyzed according to the Kaplan-Meier method, and differences between survival distributions were assessed with the log-rank test. Univariate and multivariate models were computed using Cox proportional-hazards regression (R package survival) (see Text S1 for details).
Results
Unsupervised Analysis of Gene Expression Profiles Revealed Six Subtypes of Colon Cancer
Consensus unsupervised analysis of the GEP data from the 443 samples of the discovery set revealed six clusters of samples based on the most variant probe sets (n = 1,459): C1 (n = 95, 21%), C2 (n = 83, 19%), C3 (n = 56, 13%), C4 (n = 46, 10%), C5 (n = 118, 27%), and C6 (n = 45, 10%) (Figure 1; Table S2). The consensus matrix showed that C2, C3, C4, and C6 appeared as well-individualized clusters, whereas there was more classification overlap between C1 and C5 (Figure 1A). Based on cluster expression centroid classification and the gene expression heatmap (Figure 1B and 1C), cluster C4 appeared to be the most distinct. The other clusters subdivided into C2 and C3 on one side of the cluster expression centroid classification (Figure 1B), and C6, C5, and C1 on the other. The GEPs of C1 and C5 showed overlap but displayed slightly distinct gene deregulations. This was confirmed in the supervised selection of the cluster-discriminant probe sets shown in the gene expression heatmap in Figure S2 and detailed in Table S3.
Fig. 1. Unsupervised gene expression analysis of the discovery set of 443 colon cancers. 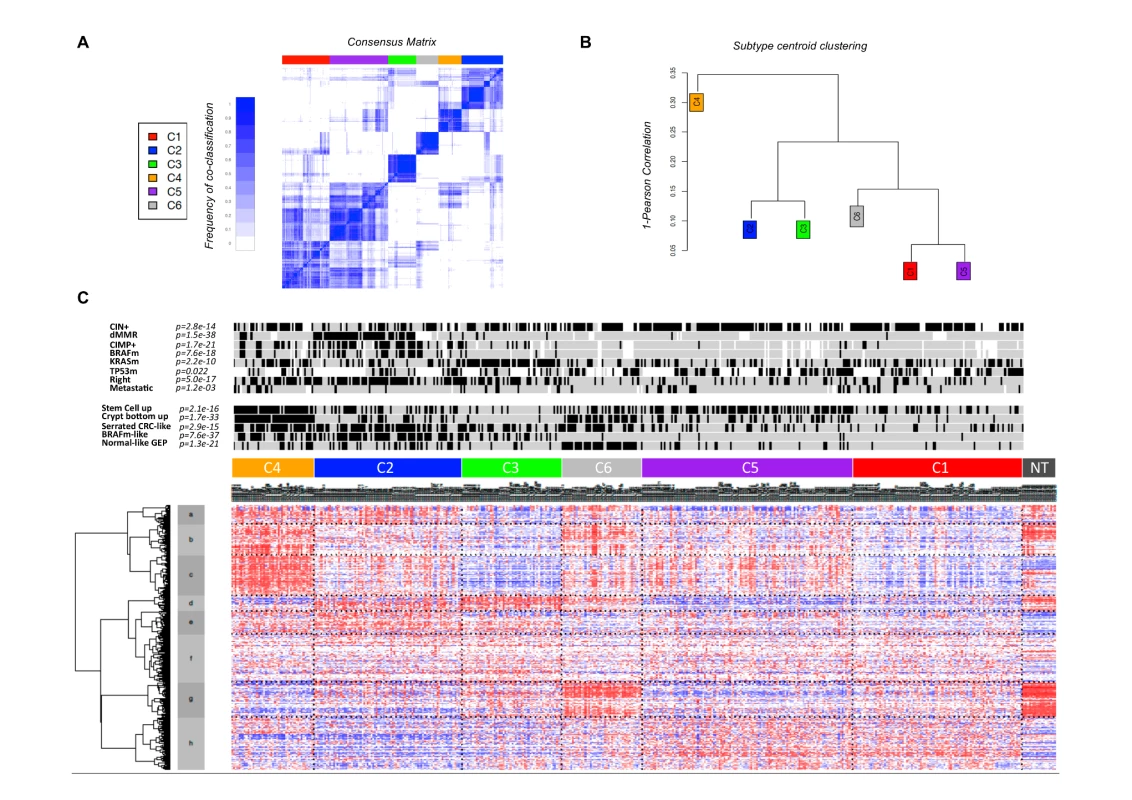
(A) Consensus matrix heatmap defining six clusters of samples for which consensus values range from 0 (in white, samples never clustered together) to 1 (dark blue, samples always clustered together). (B) Distance between clusters according to the hierarchical clustering of the 1,459 probe sets based on the centroids of each cluster. (C) GEP heatmap of the 1,459 probe sets ordered by subtype, with annotations associated with each subtype. Clinical and Molecular Relevance of Colon Cancer Subtypes
Associations with anatomoclinical and DNA alterations data are shown in Figures 1C and S3A and in Table S4. Tumors classified as C1, C5, and C6 were more frequently CIN+, CIMP−, TP53-mutant, and distal (p<0.001), without any other molecular or clinicopathological features able to discriminate these three clusters clearly. Tumors classified as C2, C4, and C3 were more frequently CIMP+ (59%, 34%, and 18%, respectively, versus <5% in other clusters) and proximal. C2 was enriched for dMMR (68%) and BRAF-mutant tumors (40%). C3 was enriched for KRAS-mutant tumors (87%). No association between clusters and TNM stage was found, except enrichment for metastatic (31%) tumors in C4.
The analyses of CGH arrays revealed that CIN+ samples shared a typical DNA copy alteration pattern including +7, −8p, +8q, +13q, −17p, −18, +20q. Differences between subtypes mainly reflected their relative content of CIN+ samples. However, some specific alterations were observed for the two CIN subtypes, C5 (+2, +11, +17q) and C1 (−10q, −14q, −15q) (Figure S4).
Signaling Pathways Associated with Colon Cancer Subtypes
We analyzed cancer-related signaling pathways from the Kyoto Encyclopedia of Genes and Genomes database for specific deregulation in each subtype signature (Figure 2). As expected, up-regulated immune system and cell growth pathways were found in C2, the subtype enriched for dMMR tumors. C4 and C6 both showed down-regulation of cell growth and death pathways and up-regulation of the epithelial–mesenchymal transition/motility pathways. Most signaling pathways were down-regulated in C1 and C3. In C5, cell communication, Wnt, and metabolism pathways were up-regulated. In C1, cell communication and immune pathways were down-regulated.
Fig. 2. Signaling pathways associated with each molecular subtype. 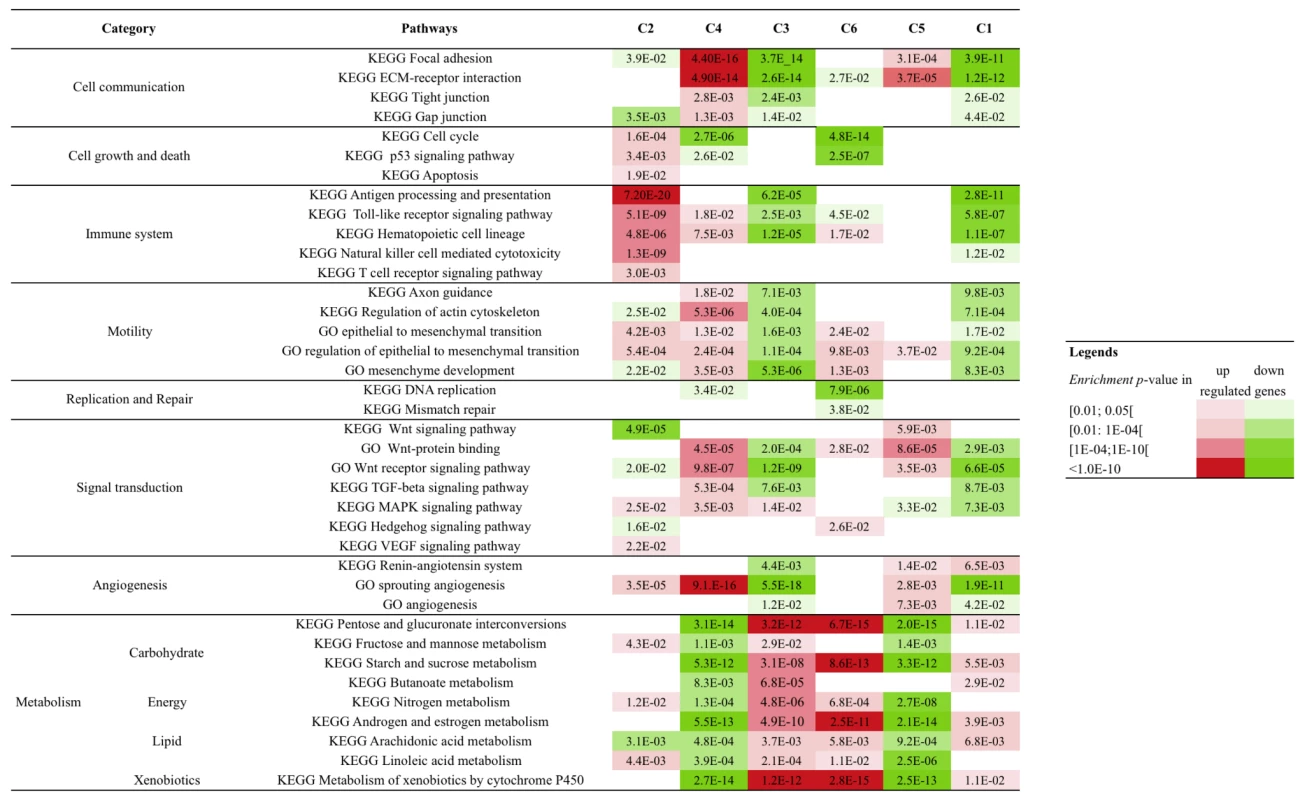
The enrichment of Kyoto Encyclopedia of Genes and Genomes (KEGG) and GeneOntology (GO) pathways and gene sets related to cancer hallmarks was tested in each subtype signature (1,000 top differentially up- and down-expressed genes, separately). The hypergeometric test p-values for enrichment in up- and down-regulated signatures are indicated in red and green, respectively. ECM, extracellular matrix. Exploratory Analysis of Cell and Precursor Origins of the Subtypes
These six molecular subtypes were further investigated using GEP data from NT and previously published supervised signatures based on DNA alterations and cellular phenotypes to explore the subtype origins. Based on the growing amount of data suggesting that cancer is closely linked to stem cells, a mouse-derived intestinal stem cell signature [24] and a human colon top and bottom crypt signature were selected and applied to our GEP data [25]. C4 appeared highly enriched for tumors displaying “stem cell phenotype–like” GEPs (91%) and up-regulating of the bottom crypt signature (96%). (Figure S3A). This finding was consistent with the pathways specifically deregulated in C4 (cell cycle pathway down-regulated and cell communication pathway up-regulated).
As previously described for breast cancer [23], we also investigated the existence of a “normal-like” subtype using the GEP centroid from NT samples. C6 was enriched for normal-like GEP tumors, although 86% of them were CIN+.
Serrated CC, in contrast to conventional CC, may arise through a recently introduced serrated neoplasia pathway [27]. We therefore applied the supervised signature, described by Laiho et al. [27], comparing gene expression of serrated to conventional CC to our GEP data. Most of the tumors classified as C2, C3, C4, and C6 displayed a “serrated CC phenotype–like” GEP, whereas those in C1 and C5 displayed a “conventional CC phenotype–like” GEP. A strong association between BRAF mutations and the serrated adenoma pathway has been reported [28], and a BRAF-mutant-like supervised signature has been described by Popovici et al. [26] that identifies a BRAF wild-type subgroup, 30% of which were KRAS mutants and 13% of which were double wild-type CC. This signature was also applied to our GEP data: subtypes C2, C3, and C4 were enriched in BRAF-mutant-like GEP tumors.
A schematic summary of the subtype characteristics is shown in Figure 3. The six subtypes were named according their main respective biological characteristic as follows: C1, “CINImmuneDown”; C2, “dMMR”; C3, “KRASm” (for “KRAS-mutant”); C4 “CSC” (for “cancer stem cell”); C5, “CINWntUp”; and C6, “CINnormL”.
Fig. 3. Summary of the main characteristics of the six subtypes. 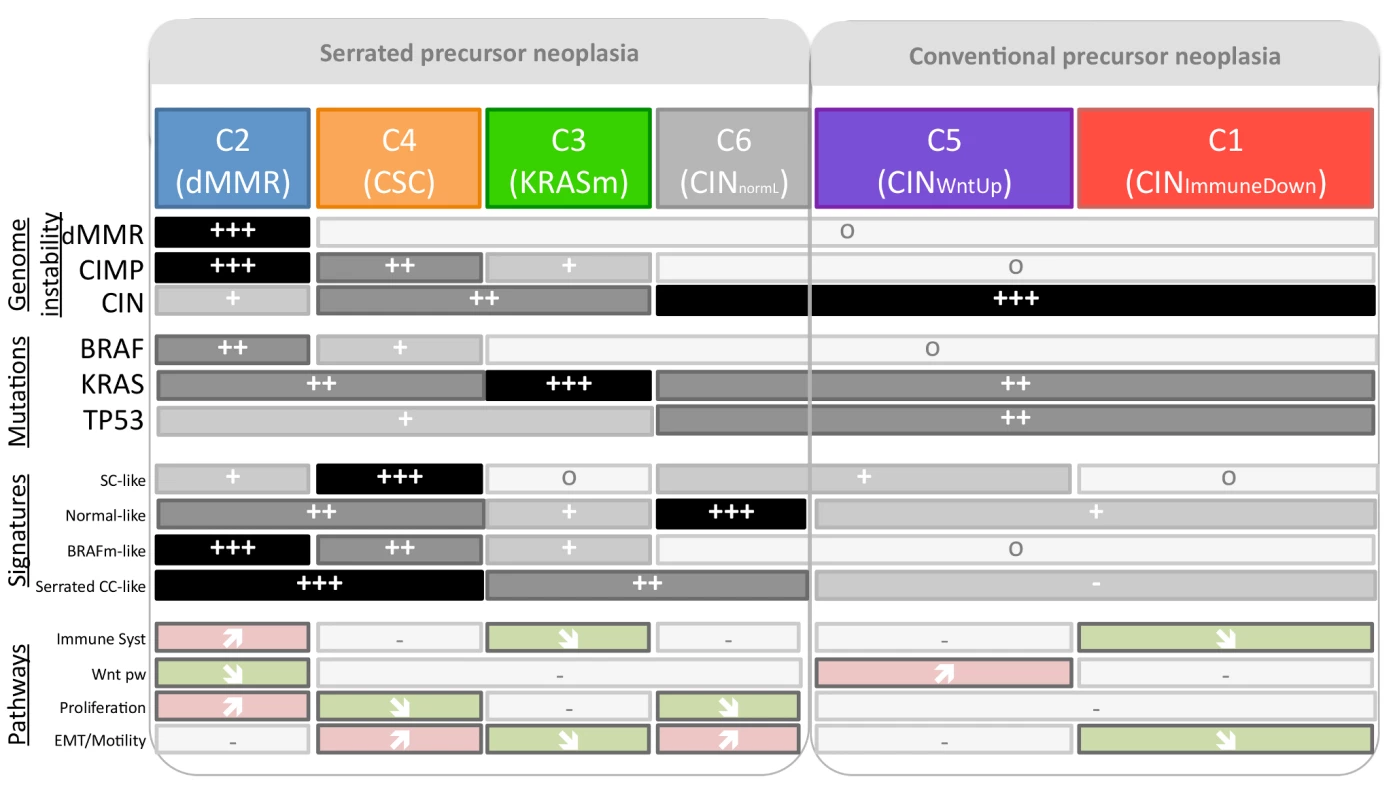
Symbols correspond to the relative frequency within the subtype (o: very low frequencies [∼0%]; +++: very high frequencies; +/++: intermediate frequencies), and arrows indicate significant enrichment of subtype up- and down-regulated genes in most of the pathways of the given category. EMT, epithelial–mesenchymal transition; SC, stem cell; Wnt pw, Wnt pathway. Validation of the Subtypes across Nine Colon Cancer Datasets
To validate our six-subtype classification, a 57-gene centroid classifier was built from the discovery set by a 10-fold cross-validation approach (<5% misclassification; Figure S5; Table S5). We applied this signature to the Affymetrix validation set of 1,029 samples (Table 1). All subtypes were found in the same proportions as in the discovery set, and the main associations between the different clusters and anatomoclinical/DNA/GEP characteristics described above were confirmed (Figures S2B and S3B), except for the enrichment of C4 with BRAF-mutant and stage IV tumors. When applied to the Agilent TCGA dataset (n = 152) [13], the molecular and clinical characteristics of the subtypes were all confirmed (Figure S3C). To further validate the six-subtype classification in the validation dataset, we performed the same consensus clustering approach with the whole validation set; the subtypes generated were highly concordant with the six assigned subtypes (Chi-squared test, p<10−16).
Prognostic Value of the Six-Subtype Classification
Further investigation of the clinical relevance of our classification included a prognostic analysis based on RFS restricted to stage II and III tumors. The prognosis of each of our six subtypes in the discovery set (n = 359) differed, but not significantly so, with patients whose tumors were classified as C4 and C6 having a relatively poorer outcome (5-y RFS rates of 52% and 61%, respectively, compared to 70%, 77%, 65%, and 70% for C1, C2, C3, and C5, respectively; p = 0.18) (Figure 4A). The prognostic value of the six-subtype classification was significant in the validation set (n = 416) (p = 0.0009), with a worse prognosis confirmed for patients with C4 and C6 tumors (Figure 4B); The six-subtype classification was also significant for the discovery and the validation sets combined (p = 0.0003) (Figure 4C). To compare the prognostic value of our classification to other prognostic covariates, we recoded our classification by combining C4 and C6 into a single high-risk group, versus all other subtypes as the low-risk group. This binary classification led to an even stronger association of the high-risk group versus the low-risk group with RFS (hazard ratio [HR] 1.7, 95% CI 1.1–2.6, p = 0.014, in the discovery set; HR 2.3, 95% CI 1.5–3.5, p = 0.00012, in the validation set; HR 2, 95% CI 1.5–2.7, p = 7.1×10−6, in the overall dataset) (Figures 4D and S6) and remained an independent prognostic factor, together with TNM stage, in the multivariate analysis (discovery and validation sets analyzed separately and merged) (Tables 2 and S6). The binary classification also remained an independent prognostic factor (p<0.01) when common DNA alterations (MMR status, CIMP, and BRAF and KRAS mutations) were added to the model (Table S7).
Fig. 4. Kaplan-Meier relapse-free survival. 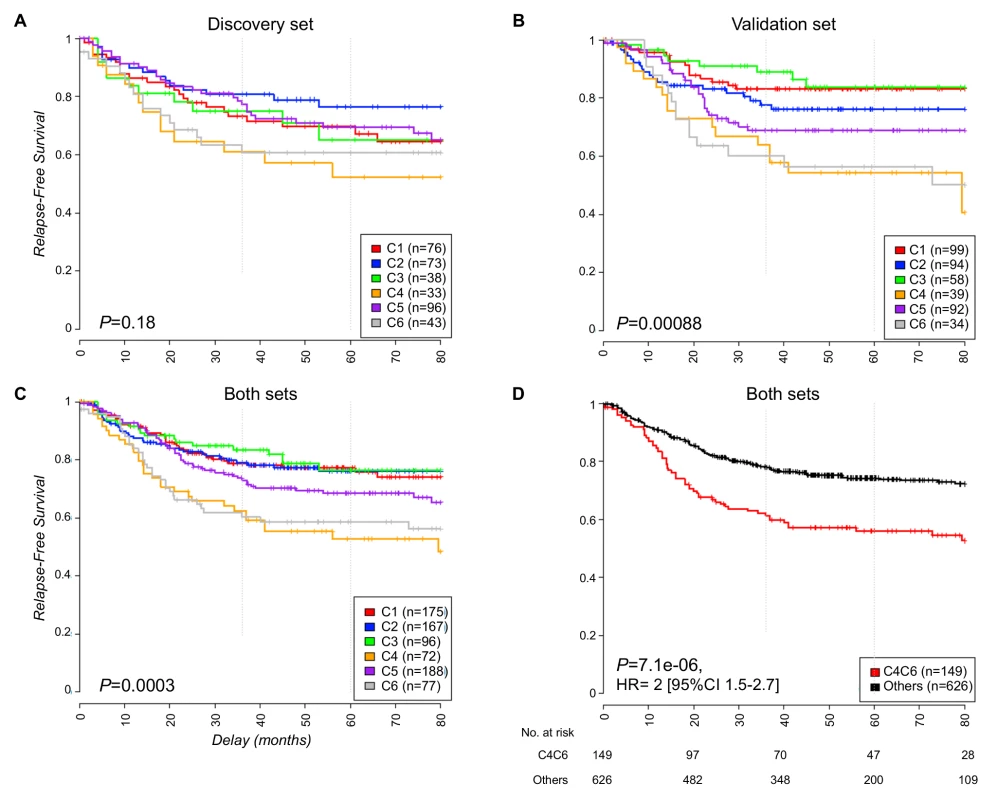
This figure shows RFS in (A) the discovery dataset, (B) the validation dataset, (C) the overall dataset, and (D) the overall dataset for C4 and C6 subtypes combined versus the other subtypes; the numbers at risk on the time axis are given. Tab. 2. Univariate and multivariate analyses of relapse-free survival according to clinical annotations, the six-subtype classification, and the Oncotype DX prognostic classifier in the overall dataset. 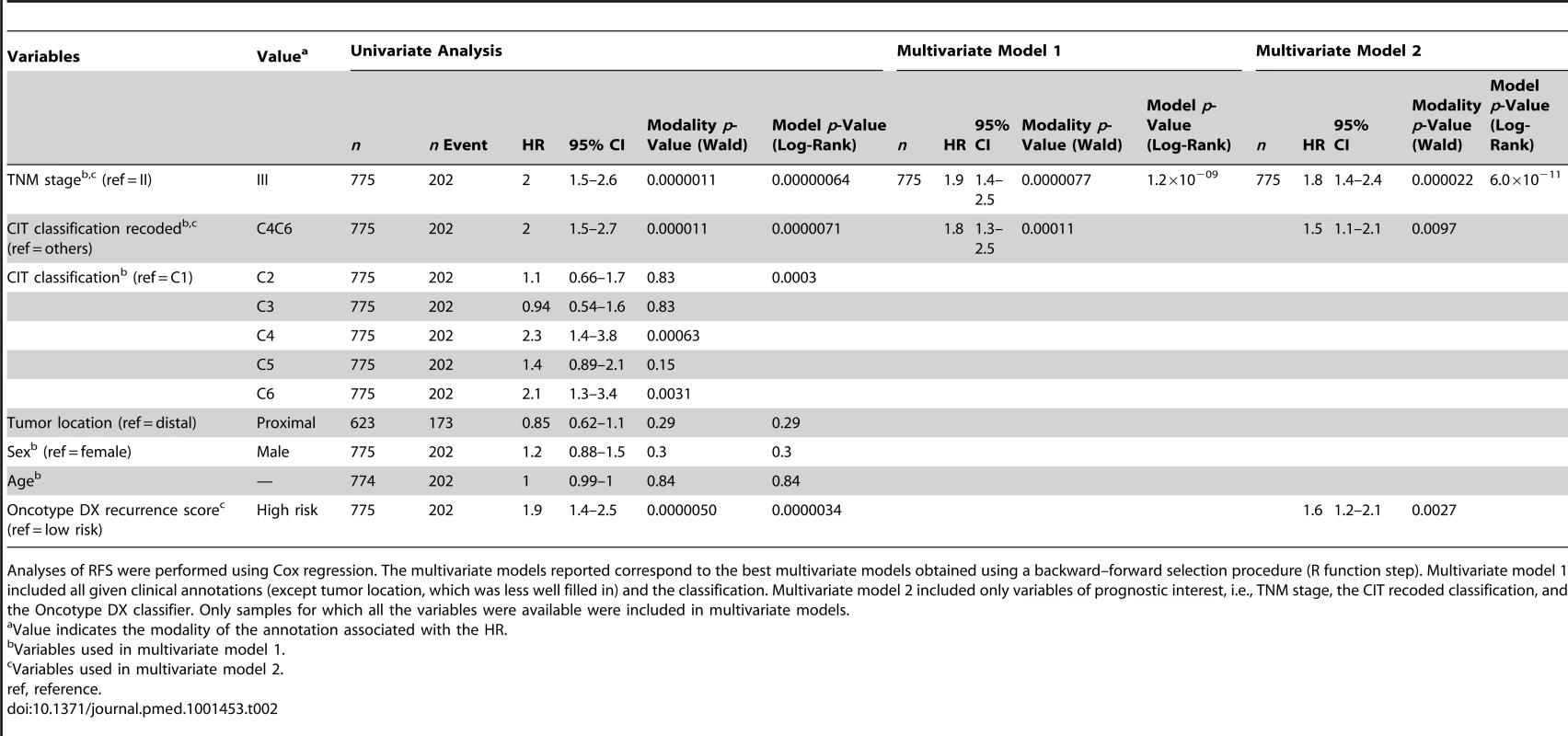
Analyses of RFS were performed using Cox regression. The multivariate models reported correspond to the best multivariate models obtained using a backward–forward selection procedure (R function step). Multivariate model 1 included all given clinical annotations (except tumor location, which was less well filled in) and the classification. Multivariate model 2 included only variables of prognostic interest, i.e., TNM stage, the CIT recoded classification, and the Oncotype DX classifier. Only samples for which all the variables were available were included in multivariate models. Prognostic Classifiers within Subtypes
The Oncotype DX recurrence score [8] is an emerging prognostic classifier, and we attempted to assess its prognostic value with our data. This score had prognostic value in both the discovery and validation sets, and in the overall dataset (p = 3.4×10−6; Figure S6). In particular, 97% of the C4 samples were classified as high risk by the Oncotype DX score. However, this score was not prognostic for all of the subtypes (Figure S7). In a multivariate stepwise analysis, both our recoded classification and the Oncotype DX score remained independently prognostic, together with TNM stage (Table 2).
We also attempted an exploratory analysis of the signature described by Salazar et al. [7] by investigating 17 of the 18 probe sets available on the Affymetrix U133 Plus 2.0 chips. We found no significant prognostic value of this 17-gene expression signature in our series (Figure S6).
Discussion
Using a large comprehensively characterized multicenter cohort of CC patients, we identified six robust molecular subtypes of CC individualized by distinct clinicobiological characteristics. Importantly, this six-subtype classification was validated in nine independent datasets. Furthermore, classification into high - and low-risk subtypes was of prognostic value.
Although retrospective, our cohort was very representative of the clinicopathological characteristics and common DNA alteration frequencies observed in the population of patients with CC.
Our findings clearly demonstrate that anatomoclinical factors and common DNA alterations alone are helpful for highlighting subtype characteristics, but they are not sufficient to define boundaries between subtypes and to describe the molecular heterogeneity of CC. Our classification successfully identified the dMMR tumor subtype, and also individualized five other distinct subtypes among pMMR tumors, including three CIN+ CIMP − subtypes representing slightly more than half of the tumors. As expected, mutation of BRAF was associated with the dMMR subtype, but was also frequent in the C4 CIMP+ poor prognosis subtype. TP53 - and KRAS-mutant tumors were found in all the subtypes; nevertheless, the C3 subtype, highly enriched in KRAS-mutant CC, was individualized and validated, suggesting a specific role of this mutation in this particular subgroup of CC. There was no significant association between our classification and pathological stage, suggesting that tumor subtype is established at the initial stages.
Exploratory analysis of each subtype GEP with previously published supervised signatures and relevant deregulated signaling pathways improved the biological relevance of the classification. Indeed, this analysis suggested that different types of CC may arise from distinct cell origins, and distinguished between the two main pathways, defined as the serrated and the conventional precursor neoplasia pathways. Interestingly, we not only individualized the dMMR subtype among the serrated precursor neoplasia subtypes, but also within the C4 CSC and the C3 KRASm subtypes. This finding is consistent with the serrated polyp classification showing two main groups: the sessile serrated adenomas, commonly associated with dMMR tumors, and the traditional serrated adenomas, commonly associated with KRAS-mutant tumors [29]. However, the proportion of serrated precursor neoplasia tumors that we found was higher than expected, indicating that further pathological investigations are required.
Another interesting finding is the reproducible association between the stem cell signature and the poor prognosis C4 subtype. Almost half of the top genes deregulated in C4—including secreted frizzled-related protein 2 (SFRP2), described as a key factor in stem cell regulation [30] and belonging to the Frizzled gene family, and growth arrest-specific 1 (GAS1)—were included in the poor prognosis cluster signature reported by Oh et al. [31]; these genes may therefore be markers of the aggressiveness of CC cells and may constitute potential therapeutic targets.
The C6 CINnormL subtype was more difficult to characterize; it belongs to the CIN+ subgroup but has a GEP and RFS that are distinct from those of the other two CIN subtypes. Several genes up-regulated in C6, in particular carbonic anhydrase II (CA2) and solute carrier family 4, sodium bicarbonate cotransporter, member 4 (SLC4A4), were also included in the prognostic classifier described by Lin et al [32].
The two other CIN subtypes, C1 and C5, were more difficult to distinguish from each other. They show common clinical and DNA alteration characteristics. They share some gene expression patterns, leading to lower co-classification rates than for the other subtypes. Moreover, these two subtypes are combined if the number of clusters is set to five instead of six. As a result, the division of C1 and C5 into two distinct subtypes can be questioned (Figure S8). However, the C1 and C5 subtypes are also clearly associated with distinct gene expression signatures (Table S3; Figure S2) and display specific pathway deregulation (immunity and epithelial–mesenchymal transition pathways; Figure 2). In addition, only four out of 507 samples in the validation set classified as subtype C1 or C5 had a mixed assignment C1/C5, as a result of being close to both the C1 and C5 centroids (see Text S1). Altogether, these observations supported these two clusters being representative of two distinct molecular entities.
The biological relevance of our subtypes was highlighted by significant differences in prognosis. In our unsupervised hierarchical clustering, patients whose tumors were classified as C4 or C6 had poorer RFS than the other patients. Thus, our study, like others [7],[31], supports the idea that the unsupervised analysis of transcripts in primary tumors yields information of prognostic value. The prognostic value of our signature was statistically significant in the validation and the overall datasets, independently of TNM stage, with a worse prognosis confirmed for C4 and C6 subtypes. Subtype C4 was enriched in CIMP+ BRAF-mutant tumors and may correspond to the poor prognostic cluster reported by Salazar et al. containing the same proportion of BRAF-mutant tumors [7].
Prognostic analyses based solely on common DNA alterations can distinguish between risk groups, but are still inadequate, as most CCs are pMMR CIMP − BRAFwt (75% in our series; data not shown). Indeed, the markers BRAF-mutant, CIMP+, and dMMR may be useful for classifying a small proportion of cases, but are uninformative for a large number of patients. This was illustrated in the study by Salazar et al. in which BRAF mutation was found in both good and poor outcome clusters, but was rare in the intermediate prognosis cluster used to build the ColoPrint prognostic classifier [7].
The ColoPrint and Oncotype DX prognostic classifiers were developed recently to improve risk prediction in early-stage CRC [7],[8]. ColoPrint was validated in three independent datasets of stage II–IIIA CC, and the robustness of the signature is currently being evaluated prospectively [33],[34]. The corresponding 17 probe sets available on Affymetrix chips did not identify risk groups in our series (data not shown). Oncotype DX has been validated as a prognostic score in the QUASAR and CALGB9581 trials, and more recently in an independent cohort of patients with stage III CC [35]–[37]. Although not identified by a genome-wide gene expression approach, the Oncotype DX score's prognostic value was confirmed in our overall stage II–III CC dataset but not in every subtype: it had prognostic value for the C3, C4, and C6 subtypes, and marginally in C5; it did not have prognostic value in C1 and C2, which represent 44% of our overall dataset. Our classification added prognostic information that remained significant in the multivariate analysis adjusted for TNM and Oncotype DX score. This suggests that the “one size fits all” prognostic signature approach can be difficult to apply because of the heterogeneity of CC. This may explain, in part, the poor concordance of GEP prognostic signatures in CC [38].
Our multivariate analysis has some limitations. In particular, some established predictors of CC prognosis, notably tumor grade and number of nodes examined, were not included because this information was not available for a substantial proportion of cases [39]. Thus, the significance and robustness of the signature as a prognostic classification requires further confirmation, ideally with large prospective patient cohorts included in adjuvant trials.
In conclusion, we report a new classification of CC into six robust molecular subtypes that arise through distinct biological pathways and represent novel prognostic subgroups. Our study clearly demonstrates that these gene signatures reflect the molecular heterogeneity of CC. This classification therefore provides a basis for the rational design of robust prognostic signatures for stage II–III CC and for identifying specific, potentially targetable markers for the different subtypes.
Supporting Information
Zdroje
1. GreenleeRT, MurrayT, BoldenS, WingoPA (2000) Cancer statistics, 2000. CA Cancer J Clin 50 : 7–33.
2. American Joint Committee on Cancer (1997) AJCC cancer staging manual, 5th edition. Philadelphia: Lippincott-Raven.
3. PopatS, HubnerR, HoulstonRS (2005) Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 23 : 609–618.
4. HutchinsG, SouthwardK, HandleyK, MagillL, BeaumontC, et al. (2011) Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 29 : 1261–1270.
5. WangY, JatkoeT, ZhangY, MutchMG, TalantovD, et al. (2004) Gene expression profiles and molecular markers to predict recurrence of Dukes' B colon cancer. J Clin Oncol 22 : 1564–1571.
6. EschrichS, YangI, BloomG, KwongKY, BoulwareD, et al. (2005) Molecular staging for survival prediction of colorectal cancer patients. J Clin Oncol 23 : 3526–3535.
7. SalazarR, RoepmanP, CapellaG, MorenoV, SimonI, et al. (2011) Gene expression signature to improve prognosis prediction of stage II and III colorectal cancer. J Clin Oncol 29 : 17–24.
8. O'ConnellMJ, LaveryI, YothersG, PaikS, Clark-LangoneKM, et al. (2010) Relationship between tumor gene expression and recurrence in four independent studies of patients with stage II/III colon cancer treated with surgery alone or surgery plus adjuvant fluorouracil plus leucovorin. J Clin Oncol 28 : 3937–3944.
9. JassJR (2007) Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology 50 : 113–130.
10. ShenL, ToyotaM, KondoY, LinE, ZhangL, et al. (2007) Integrated genetic and epigenetic analysis identifies three different subclasses of colon cancer. Proc Natl Acad Sci U S A 104 : 18654–18659.
11. KangGH (2011) Four molecular subtypes of colorectal cancer and their precursor lesions. Arch Pathol Lab Med 135 : 698–703.
12. HinoueT, WeisenbergerDJ, LangeCP, ShenH, ByunHM, et al. (2012) Genome-scale analysis of aberrant DNA methylation in colorectal cancer. Genome Res 22 : 271–282.
13. Cancer Genome Atlas Network (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487 : 330–337.
14. LièvreA, BachetJB, BoigeV, CayreA, Le CorreD, et al. (2008) KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol 26 : 374–379.
15. CabelguenneA, BlonsH, de WaziersI, CarnotF, HoullierAM, et al. (2000) p53 alterations predict tumor response to neoadjuvant chemotherapy in head and neck squamous cell carcinoma: a prospective series. J Clin Oncol 18 : 1465–1473.
16. BolandCR, ThibodeauSN, HamiltonSR, SidranskyD, EshlemanJR, et al. (1998) A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58 : 5248–5257.
17. WeisenbergerDJ, SiegmundKD, CampanM, YoungJ, LongTI, et al. (2006) CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet 38 : 787–793.
18. de ReynièsA, AssiéG, RickmanDS, TissierF, GroussinL, et al. (2009) Gene expression profiling reveals a new classification of adrenocortical tumors and identifies molecular predictors of malignancy and survival. J Clin Oncol 27 : 1108–1115.
19. IrizarryRA, BolstadBM, CollinF, CopeLM, HobbsB, et al. (2003) Summaries of Affymetrix GeneChip probe level data. Nucleic Acids Res 31: e15.
20. JohnsonWE, LiC, RabinovicA (2007) Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 8 : 118–127.
21. GuedjM, MarisaL, de ReyniesA, OrsettiB, SchiappaR, et al. (2012) A refined molecular taxonomy of breast cancer. Oncogene 31 : 1196–1206.
22. MontiS, TamayoP, MesirovJ, GolubT (2003) Consensus clustering: a resampling-based method for class discovery and visualization of gene expression microarray data. Mach Learn 52 : 91–118.
23. SorlieT, TibshiraniR, ParkerJ, HastieT, MarronJS, et al. (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A 100 : 8418–8423.
24. Merlos-SuárezA, BarrigaFM, JungP, IglesiasM, CéspedesMV, et al. (2011) The intestinal stem cell signature identifies colorectal cancer stem cells and predicts disease relapse. Cell Stem Cell 8 : 511–524.
25. KosinskiC, LiVS, ChanAS, ZhangJ, HoC, et al. (2007) Gene expression patterns of human colon tops and basal crypts and BMP antagonists as intestinal stem cell niche factors. Proc Natl Acad Sci U S A 104 : 15418–15423.
26. PopoviciV, BudinskaE, TejparS, WeinrichS, EstrellaH, et al. (2012) Identification of a poor-prognosis BRAF-mutant-like population of patients with colon cancer. J Clin Oncol 30 : 1288–1295.
27. LaihoP, KokkoA, VanharantaS, SalovaaraR, SammalkorpiH, et al. (2007) Serrated carcinomas form a subclass of colorectal cancer with distinct molecular basis. Oncogene 26 : 312–320.
28. SnoverDC (2011) Update on the serrated pathway to colorectal carcinoma. Hum Pathol 42 : 1–10.
29. LiangJJ, BissettI, KaladyM, BennetA, ChurchJM (2012) Importance of serrated polyps in colorectal carcinogenesis. ANZ J Surg E-pub ahead of print. doi:10.1111/j.1445-2197.2012.06269.x.
30. AlfaroMP, PagniM, VincentA, AtkinsonJ, HillMF, et al. (2008) The Wnt modulator sFRP2 enhances mesenchymal stem cell engraftment, granulation tissue formation and myocardial repair. Proc Natl Acad Sci U S A 105 : 18366–18371.
31. OhSC, ParkYY, ParkES, LimJY, KimSM, et al. (2011) Prognostic gene expression signature associated with two molecularly distinct subtypes of colorectal cancer. Gut 61 : 1291–1298.
32. LinYH, FriederichsJ, BlackMA, MagesJ, RosenbergR, et al. (2007) Multiple gene expression classifiers from different array platforms predict poor prognosis of colorectal cancer. Clin Cancer Res 13 : 498–507.
33. Salazar R, Tabernero J, Moreno V, Nitsche U, Bachleitner-Hofmann T, et al.. (2012) Validation of a genomic classifier (ColoPrint) for predicting outcome in the T3-MSS subgroup of stage II colon cancer patients [abstract 3510]. American Society of Clinical Oncology Annual Meeting; 1–5 Jun 2012; Chicago, Illinois, US.
34. (2011) A prospective study for the assessment of recurrence risk in stage II colon cancer patients using ColoPrint (PARSC). ClinicalTrials.gov: NCT00903565. Available: http://clinicaltrials.gov/ct2/show/NCT00903565. Accessed 16 April 2013.
35. GrayRG, QuirkeP, HandleyK, LopatinM, MagillL, et al. (2011) Validation study of a quantitative multigene reverse transcriptase-polymerase chain reaction assay for assessment of recurrence risk in patients with stage II colon cancer. J Clin Oncol 29 : 4611–4619.
36. VenookAP, NiedzwieckiD, LopatinM, LeeM, FriedmanPN, et al. (2011) Validation of a 12-gene colon cancer recurrence score (RS) in patients (pts) with stage II colon cancer (CC) from CALGB 9581 [abstract]. 2011 ASCO Annual Meeting Proceedings (Post-Meeting Edition). J Clin Oncol 29(May 20 Suppl): 3518.
37. O'ConnellM, LeeM, LopatinM, YothersG, Clark-LangoneK, et al. (2012) Validation of the 12-gene colon cancer recurrence score (RS) in NSABP C07 as a predictor of recurrence in stage II and III colon cancer patients treated with 5FU/LV (FU) and 5FU/LV+oxaliplatin (FU+Ox) [abstract]. 2012 ASCO Annual Meeting Proceedings (Post-Meeting Edition). J Clin Oncol 30(May 20 Suppl): 3512.
38. Roth A, Di Narzo AF, Tejpar S, Bosman F, Popovici V, et al.. (2012) Validation of two gene-expression risk scores in a large colon cancer cohort and contribution to an improved prognostic method [abstract 3509]. American Society of Clinical Oncology Annual Meeting; 1–5 Jun 2012; Chicago, Illinois, US.
39. WeiserMR, GönenM, ChouJF, KattanMW, SchragD (2011) Predicting survival after curative colectomy for cancer: individualizing colon cancer staging. J Clin Oncol 29 : 4796–4802.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 5- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Nutraceutikum Armolipid Plus podle klinických důkazů zlepšuje lipidový profil − metaanalýza
- Snižuje terapie betablokátory kardiovaskulární benefit aerobního cvičení u pacientů s arteriální hypertenzí?
-
Všechny články tohoto čísla
- Measuring Coverage in MNCH: Challenges and Opportunities in the Selection of Coverage Indicators for Global Monitoring
- Measuring Coverage in MNCH: Tracking Progress in Health for Women and Children Using DHS and MICS Household Surveys
- Measuring Coverage in MNCH: Population HIV-Free Survival among Children under Two Years of Age in Four African Countries
- Tobacco Company Efforts to Influence the Food and Drug Administration-Commissioned Institute of Medicine Report An Analysis of Documents Released through Litigation
- Irreconcilable Conflict: The Tobacco Industry and the Public Health Challenge of Tobacco Use
- Providing Impetus, Tools, and Guidance to Strengthen National Capacity for Antimicrobial Stewardship in Viet Nam
- Measuring Coverage in MNCH: New Findings, New Strategies, and Recommendations for Action
- Grand Challenges: Integrating Maternal Mental Health into Maternal and Child Health Programmes
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
- Measuring Coverage in MNCH: Current Indicators for Measuring Coverage of Diarrhea Treatment Interventions and Opportunities for Improvement
- Measuring Coverage in MNCH: Evaluation of Community-Based Treatment of Childhood Illnesses through Household Surveys
- Measuring Coverage in MNCH: Accuracy of Measuring Diagnosis and Treatment of Childhood Malaria from Household Surveys in Zambia
- Grand Challenges: Integrating Mental Health Care into the Non-Communicable Disease Agenda
- Integrating Global and National Knowledge to Select Medicines for Children: The Ghana National Drugs Programme
- Grand Challenges: Integrating Mental Health Services into Priority Health Care Platforms
- Disability Transitions and Health Expectancies among Adults 45 Years and Older in Malawi: A Cohort-Based Model
- Comparative Efficacy of Seven Psychotherapeutic Interventions for Patients with Depression: A Network Meta-Analysis
- Measuring Coverage in MNCH: Design, Implementation, and Interpretation Challenges Associated with Tracking Vaccination Coverage Using Household Surveys
- Measuring Coverage in MNCH: A Prospective Validation Study in Pakistan and Bangladesh on Measuring Correct Treatment of Childhood Pneumonia
- Contribution of and Smoking Trends to US Incidence of Intestinal-Type Noncardia Gastric Adenocarcinoma: A Microsimulation Model
- Carriage of in the Upper Respiratory Tract of Symptomatic and Asymptomatic Children: An Observational Study
- Setting Research Priorities to Reduce Mortality and Morbidity of Childhood Diarrhoeal Disease in the Next 15 Years
- Grand Challenges: Improving HIV Treatment Outcomes by Integrating Interventions for Co-Morbid Mental Illness
- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Effect of Facilitation of Local Maternal-and-Newborn Stakeholder Groups on Neonatal Mortality: Cluster-Randomized Controlled Trial
- Intimate Partner Violence and Population Mental Health: Why Poverty and Gender Inequities Matter
- Assessing Population Aging and Disability in Sub-Saharan Africa: Lessons from Malawi?
- The Paradox of Mental Health: Over-Treatment and Under-Recognition
- Measuring Coverage in MNCH: Determining and Interpreting Inequalities in Coverage of Maternal, Newborn, and Child Health Interventions
- Measuring Coverage in MNCH: Total Survey Error and the Interpretation of Intervention Coverage Estimates from Household Surveys
- Measuring Coverage in MNCH: Indicators for Global Tracking of Newborn Care
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



