-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaNoncommunicable Diseases: A Globalization of Disparity?
article has not abstract
Published in the journal: . PLoS Med 12(7): e32767. doi:10.1371/journal.pmed.1001859
Category: Editorial
doi: https://doi.org/10.1371/journal.pmed.1001859Summary
article has not abstract
A year ago, the editors of PLOS Neglected Tropical Diseases and PLOS Medicine launched the PLOS Blue Marble Health Collection, subtitled “the mismatch between national wealth and population health” [1]. The term “blue marble health” (which recalls the appearance of the earth from space) was coined as a differentiator from prior conceptualizations of global health that divided the world’s population according to national economic indices [2]. The basic tenet of blue marble health is that impoverished populations living amidst wealth bear a disproportionate burden of neglected diseases, irrespective of the overall economic strength of their home country. Such an approach is increasingly relevant as differential disease burdens between wealthier countries and regions (including North America, Europe, and Japan) and lower-income countries (including many in Africa, Asia, and Central and South America), evolve through a pronounced, but uneven, economic rise across the planet that leaves pockets of intense poverty in its wake.
The concept of blue marble health grew out of a paradoxical observation by one of us (PJH) that most of the world’s neglected tropical diseases (NTDs) are found in concentrated areas where poor people live in the wealthiest economies, especially the group of 20 (G20) countries together with Nigeria [2]. A follow-up study published this week in PLOS Neglected Tropical Diseases, based on newer data released by the World Health Organization (WHO) for the year 2013, finds that at least one-half or more of the world’s helminth infections and most of the dengue fever cases are also endemic to the G20 nations and Nigeria [3].
A recent analysis, based on data from WHO and the Joint United Nations Programme on HIV/AIDS (UNAIDS), indicates that lack of protection by national economic power extends beyond the NTDs to include the so-called “big three diseases”: HIV/AIDS, tuberculosis, and malaria; overall, roughly one-half of the prevalent cases of tuberculosis and malaria in 2013 were found in the G20 and Nigeria, as were almost one-half of the people living with HIV/AIDS [4].
The policy implications of blue marble health related to infections include emphasizing the G20’s role in mass treatment of their own indigenous populations for NTDs; prevention and appropriate screening for HIV, TB and malaria; and committing resources to conduct research and development (R&D) [5]. The need for such a policy is based partly on studies that point to disproportionately small contributions by the BRICS (i.e., Brazil, Russia, India, China, and South Africa) and other G20 countries towards supporting health R&D globally [6].
If diseases long associated with poor countries, such as NTDs and other infections, are increasing among poor people in richer countries, what about diseases associated with rich countries? Noncommunicable diseases (NCDs), including such rich-country scourges as coronary artery disease, have for some years been increasing as causes of illness and death in low - and middle-income countries [7]. According to WHO’s Global Status Report on NCDs 2014 for the year 2012, globally approximately 38 million people died from NCDs, from a total of 56 million people who died in that year. The WHO finds that four major disease groups—cancer, cardiovascular diseases, chronic respiratory diseases, and diabetes—are responsible for 82% of the NCD-related deaths. Among them, cardiovascular diseases accounted for almost one-half of the deaths (17.5 million), followed by cancers (8.2 million), respiratory diseases such as asthma and chronic obstructive pulmonary disease (4.0 million), and diabetes (1.5 million) [8].
Are increases in NCDs limited to growing higher-income classes? In 2013, the G20 nations and Nigeria accounted for almost 90% of the global economy, as estimated by total global gross domestic product (GDP). While these nations represent the world’s economic engine, the G20 nations and Nigeria also produce most of the world’s neglected infectious diseases (including NTDs) and most of its NCDs. Shown in Table 1 is the NCD mortality for the G20 countries and Nigeria, indicating that the world’s wealthiest economies account for approximately 26.5 million deaths from NCDs, or 70% of the world’s NCD-related deaths. The age-standardized death rates clearly indicate that, among the world’s leading economic powers, a nation’s GDP by itself is a poor indicator of its inhabitants’ risk of dying from NCDs.
Tab. 1. NCD mortality estimates in G20 countries + Nigeria, 20121. 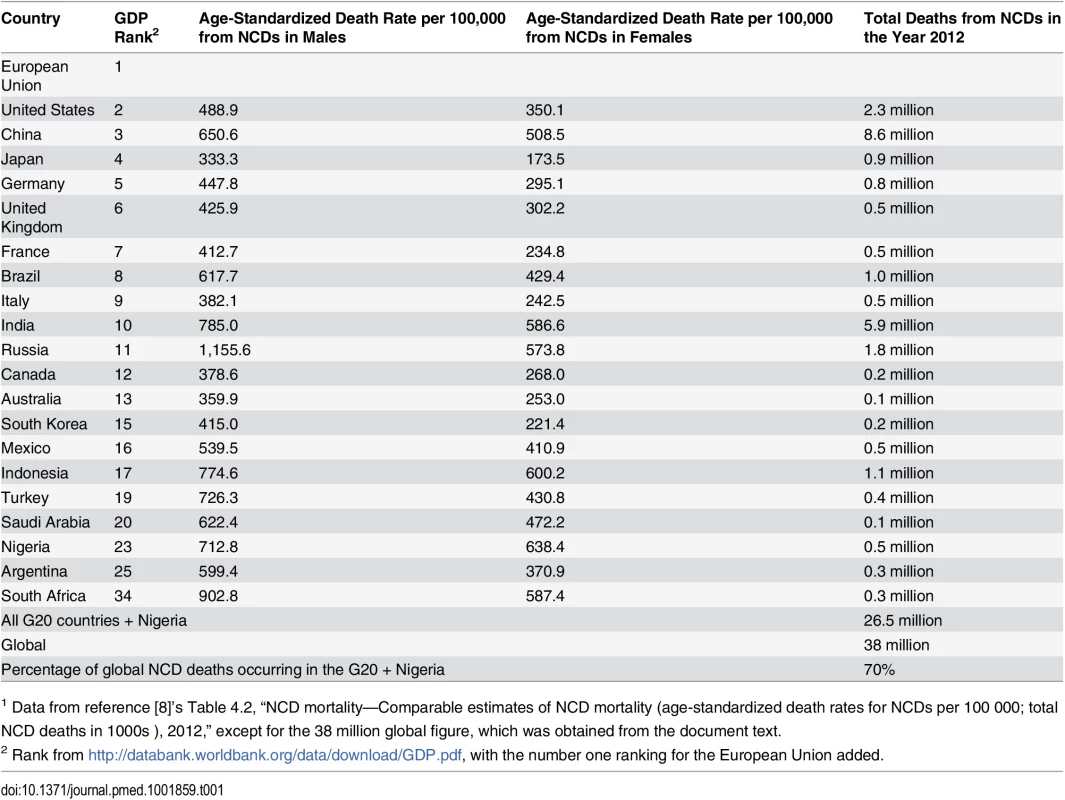
1 Data from reference [8]’s Table 4.2, “NCD mortality—Comparable estimates of NCD mortality (age-standardized death rates for NCDs per 100 000; total NCD deaths in 1000s ), 2012,” except for the 38 million global figure, which was obtained from the document text. These WHO data do not distinguish between wealthy and poor populations within the G20 nations and Nigeria. However, previous work indicates that at least some NCDs have been associated with lower, rather than higher, socioeconomic status within LMICs [9]. Moreover, NCDs are on the decline in high-income countries but rising among LMICs, where most of the world’s NCD-related deaths (especially premature deaths) now occur [8]. Taken together with these findings, the wide range of NCD mortality rates among G20 countries, with particularly high rates among non-high-income G20 countries, seems consistent with a hypothesis that the poor living among the wealthy disproportionately share the burden of NCDs globally. In other words, NCDs may be joining NTDs, HIV, TB, and malaria in following the familiar blue marble health pattern of geographical redistribution with convergence on the world’s poorest people.
These observations indicate the relevance of a blue marble health perspective in reshaping global health policy to include a spotlight on the G20 nations and Nigeria and targeting HIV/AIDS, tuberculosis, malaria, NTDs, and NCDs at future G20 summits. A specific component may include renewed commitments by these specific nations for access to health care and essential medicines for their own impoverished populations as well as those of lower-income countries. To this end, G20 nations should support the nine major targets that WHO has set to reduce global deaths from NCDs, with an overarching goal to reduce NCD deaths by one-quarter [8]. Important components include dietary and lifestyle changes, as well as access to essential medicines to control high blood sugar, high blood pressure, and other risk factors for cardiovascular diseases. In addition, there are a wide range of neglected causes of NCDs that are unique to people who live in extreme poverty [10] Ultimately, the world economic powers should also support R&D to address their own health disparities [11]. Recently, a global biomedical R&D fund has been proposed [5], which may be especially relevant to the G20 nations and Nigeria not only as supporters of improving health in less wealthy countries, but also as potential recipients of advances that will benefit the health of their own populations.
Such measures must not be enacted while failing to address poverty and other social determinants underlying the patterns that blue marble health aims to improve. As Michael Marmot and others have noted, “Social determinants are relevant to communicable and non-communicable disease alike. Health status, therefore, should be of concern to policy makers in every sector, not solely those involved in health policy” [12]. In parallel, global efforts should ensure that implementation of public health measures does not inadvertently widen health inequalities, as recently found for some cardiovascular disease prevention measures [13]. Strong economies must take responsibility for population-wide preventive action that embraces vulnerable populations now living in extreme poverty.
For research addressing the disparate burden of disease upon poor people across a variety of settings, PLOS Medicine and PLOS Neglected Tropical Diseases continue to encourage submissions to the recently updated Blue Marble Health Collection [1,14].
Zdroje
1. Blue marble health: the mismatch between national wealth and population health. PLOS Collections. http://www.ploscollections.org/article/browse/issue/info%3Adoi%2F10.1371%2Fissue.pcol.v01.i23. Accessed 25 June 2014.
2. Hotez PJ (2013) NTDs V.2.0: “Blue Marble Health”—Neglected Tropical Disease Control and Elimination in a Shifting Health Policy Landscape. PLOS Negl Trop Dis 7: e2570. doi: 10.1371/journal.pntd.0002570 24278496
3. Hotez PJ (2015) Blue marble health redux: neglected tropical diseases, and human development in the group of 20 (G20) nations and Nigeria. PLOS Negl Trop Dis 9: e3672.
4. Hotez PJ (2015) Blue Marble Health and “The Big Three Diseases”: HIV/AIDS, Tuberculosis, and Malaria. Microbes Infect. doi: 10.1016/j.micinf.2015.05.004 E-pub ahead of print.
5. Balasegaram M, Bréchot C, Farrar J, Heymann D, Ganguly N, Khor M, et al. (2015) A Global Biomedical R&D Fund and Mechanism for Innovations of Public Health Importance. PLoS Med 12(5): e1001831. doi: 10.1371/journal.pmed.1001831 25962119
6. Hotez PJ, Cohen R, Mimura C, Yamada T, Hoffman SL (2013) Strengthening mechanisms to prioritize, coordinate, finance, and execute R&D to meet health needs in developing countries. Discussion Paper, Institute of Medicine, Washington, DC. https://www.iom.edu/Global/Perspectives/2013/StrengtheningMechanismsRD.aspx
7. Sridhar D, Brolan CE, Durrani S, Edge J, Gostin LO, Hill P, et al. (2013) Recent Shifts in Global Governance: Implications for the Response to Non-communicable Diseases. PLoS Med 10(7): e1001487. doi: 10.1371/journal.pmed.1001487 23935458
8. World Health Organization (2014) Global Status Report on Non-Communicable Diseases, 2014. http://www.who.int/nmh/publications/ncd-status-report-2014/en/
9. Hosseinpour AR, Bergen N, Mendis S, Harper S, Verdes E, et al. (2012) BMC Public Health 12 : 474 doi: 10.1186/1471-2458-12-474
10. Hotez PJ, Daar AS (2008) The CNCDs and the NTDs: Blurring the Lines Dividing Noncommunicable and Communicable Chronic Diseases. PLoS Negl Trop Dis 2(10): e312. doi: 10.1371/journal.pntd.0000312 18958154
11. Hotez PJ (2014) Blue marble health: a new presidential roadmap for global poverty-related diseases. James A Baker III Institute for Public Policy, Rice University. http://bakerinstitute.org/research/blue-marble-health-new-presidential-roadmap-global-poverty-related-diseases/
12. Marmot M (2005) Social determinants of health inequalities. Lancet 365 : 1099–1104. 15781105
13. Capewell S, Graham H (2010) Will cardiovascular disease prevention widen health inequalities? PLOS Med 7(8): e1000320. doi: 10.1371/journal.pmed.1000320 20811492
14. Hotez PJ, Peiperl L (2014) Blue Marble Health: A Call for Papers. PLoS Med 11(7): e1001682. doi: 10.1371/journal.pmed.1001682 25072140
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2015 Číslo 7- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Léčba bolesti u seniorů
- Superoxidované roztoky v prevenci infekcí u dialyzovaných pacientů
- Benefity fixní kombinace tramadolu a paracetamolu v léčbě bolesti
- Flexofytol® – přírodní revoluce v boji proti osteoartróze kloubů
-
Všechny články tohoto čísla
- Noncommunicable Diseases: A Globalization of Disparity?
- The Individualised versus the Public Health Approach to Treating Ebola
- Ebola Virus Disease: Experience and Decision Making for the First Patients outside of Africa
- Risk of Adverse Pregnancy Outcomes among Women Practicing Poor Sanitation in Rural India: A Population-Based Prospective Cohort Study
- Health, Health Inequality, and Cost Impacts of Annual Increases in Tobacco Tax: Multistate Life Table Modeling in New Zealand
- Connecting the Dots: Health Information Technology Expansion and Health Disparities
- Searching for Public Health Law’s Sweet Spot: The Regulation of Sugar-Sweetened Beverages
- Glitazone Treatment and Incidence of Parkinson’s Disease among People with Diabetes: A Retrospective Cohort Study
- Individual Participant Data (IPD) Meta-analyses of Randomised Controlled Trials: Guidance on Their Use
- AA Genotype Exacerbates Effect of Diabetes on Dementia and Alzheimer Disease: A Population-Based Longitudinal Study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ebola Virus Disease: Experience and Decision Making for the First Patients outside of Africa
- Searching for Public Health Law’s Sweet Spot: The Regulation of Sugar-Sweetened Beverages
- Glitazone Treatment and Incidence of Parkinson’s Disease among People with Diabetes: A Retrospective Cohort Study
- Individual Participant Data (IPD) Meta-analyses of Randomised Controlled Trials: Guidance on Their Use
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



