-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPopulation impact of lung cancer screening in the United States: Projections from a microsimulation model
Chung Yin Kong and colleagues model the health outcomes of lung cancer screening in the US and account for reduced levels of smoking. The benefits of screening and mortality reduction will start to decline in 5 years because of reduced smoking.
Published in the journal: . PLoS Med 15(2): e32767. doi:10.1371/journal.pmed.1002506
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002506Summary
Chung Yin Kong and colleagues model the health outcomes of lung cancer screening in the US and account for reduced levels of smoking. The benefits of screening and mortality reduction will start to decline in 5 years because of reduced smoking.
Introduction
Despite more than 50 years having passed since the publication of the first Surgeon General’s Report on Smoking and Health and the expansive tobacco control efforts that have followed, lung cancer is still the leading cause of cancer-related deaths in the US [1,2]. This suggests that additional lung cancer control policies are necessary to work alongside tobacco control and cessation efforts in order to effectively reduce lung cancer deaths [3]. For example, lung cancer screening with low-dose computed tomography (CT) has been shown to improve early detection of lung cancer and reduce mortality among screened individuals [4,5]. The National Lung Screening Trial (NLST) resulted in a 20.0% reduction in lung cancer mortality for individuals at high risk of developing lung cancer when screened with low-dose CT compared to those screened with chest radiography [6]. The US Preventive Services Task Force (USPSTF) subsequently released a recommendation supporting low-dose CT screening [7], requiring private insurers to cover the cost of screening [8]. In 2015, the US Centers for Medicare and Medicaid Services (CMS) also issued a coverage determination for annual lung cancer screening with low-dose CT [9].
Several studies have utilized simulation modeling to estimate the effects of screening strategies on lung cancer mortality by following a single birth cohort over a number of years [10–13]. However, epidemiologic studies have shown that smoking behavior, as well as lung cancer risk, vary dramatically by birth cohort [14–17]. Thus, results of single birth cohort studies are not generalizable to the US at a population level. It is not known whether the screening benefit found by single-cohort simulations will remain after taking these birth cohort differences into account. The primary purpose of this study was to investigate this issue using a well-validated simulation model, the Lung Cancer Policy Model (LCPM), to estimate the impact of changing smoking prevalence on the number of lung cancer deaths, number of screening CT exams, overall mortality reduction, life-years gained, and overdiagnoses in the US at a population level using the CMS screening eligibility criteria and a realistic screening adherence rate. Additionally, we provide an estimate of the most beneficial timing for the implementation of a comprehensive lung cancer screening program.
Materials and methods
Model overview
Simulation modeling and clinical trials offer complementary methods of investigating the relationship between a healthcare intervention and outcomes. The advantage of simulation modeling is its ability to integrate currently available short-term trial data to project long-term consequences and explore a variety of “what-if” scenarios. For example, simulation modeling can explore different screening frequencies and alternative screening technologies while targeting different age, gender, and race groups. Simulation modeling can also be used to investigate topical questions in health policy discussions, such as the effect of varying rates of adherence on screening effectiveness.
The LCPM is a well-validated, comprehensive Monte Carlo microsimulation model of non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) development, progression, detection, treatment, and survival [18,19]. The LCPM was previously utilized in lung cancer screening to study varied screening eligibility criteria, which informed the recommendations for lung cancer screening by the USPSTF [7,11].
The LCPM simulates progression, detection, follow-up, treatment, and survival of individual patients using a state-transition microsimulation method [20,21]. In the LCPM, lung cancer patients can develop adenocarcinoma (including adenocarcinoma in situ), large cell carcinoma, squamous cell carcinoma, small cell carcinoma, or other lung cancer. Histologic type informs lung cancer risks, incidence rates, and disease progression rates. Natural history parameters have been established through calibration to patient-level data from the NLST, and model outputs were validated using data from the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial (PLCO) [22]. We used the US Census Bureau’s population projections to estimate future lung cancer incidence [23].
Individual-level characteristics specific to the US population, such as age of smoking initiation, cigarettes smoked per day, and age of smoking cessation, were modeled using the “smoking history generator,” provided by the National Cancer Institute’s Cancer Intervention and Surveillance Modeling Network (CISNET) (S1 Appendix) [16,17,24]. All simulated individuals (current, former, and never smokers) aged 30–84 years were followed from 2016 to 2030. In order to estimate the variability from the stochastic nature of Monte Carlo microsimulation, we completed 20 runs of the simulation and reported means and 95% confidence intervals in our results.
Key inputs for the model include characteristics of the simulated population (e.g., birth year, smoking history, and smoking-adjusted mortality risk from competing causes) and scenario-specific items (e.g., test characteristics, screening program characteristics, screen adherence and eligibility, and response rates for treatments). For additional details, the model is described in an online technical appendix under the “MGH Institute for Technology Assessment” link on the CISNET Lung Cancer Model Profiles webpage (https://www.cisnet.cancer.gov/lung/profiles.html) and in S1 Appendix.
Screening scenarios
In our evaluation of lung cancer screening using the LCPM, the control scenario was no lung cancer screening, while the comparison scenario was lung cancer screening criteria based on the CMS guidelines. Under the CMS screening criteria, current and former smokers aged 55–77 years with at least 30 pack-years of smoking history and fewer than 15 years since quitting were screened annually for lung cancer with CT. In these scenarios, CT screening was fully implemented in the year 2016 and studied up to the year 2030. Although the CMS screening guidelines were issued in early 2015 [9], we excluded the year 2015 in evaluating the screening impacts in order to capture the first full year of implementation.
Adherence is defined as the percentage of screening-eligible smokers who comply with the CMS screening guidelines. Adherent smokers are assumed to receive screening every year they are eligible, and nonadherent smokers are assumed to not receive screening. Studies of multiple programs have reported adherence rates to lung cancer screening ranging between 35% and 50%, though conclusive data on nationwide adherence were not available [25–27]. Additionally, adherence rates for more established screening programs for colorectal, breast, cervical, and prostate cancer were estimated to be 54.6%, 69.3%, 85.8%, and 46.4%, respectively, in 2010 by a national survey [28]. Given the nascent nature of the CMS lung cancer screening guidelines, it is unlikely that the adherence rate will exceed the adherence rates of these other screening programs. Therefore, in our base case analysis, we initially assumed 45% screening adherence to reasonably estimate potential benefits and harms of screening. This value represents a conservative estimate based on adherence data from more established screening programs in other cancers while also remaining within the range of observed rates in lung cancer screening studies.
Sensitivity analyses using 100% adherence and other lower adherence rates (i.e., 25% to 75%) considered the effect of screening adherence on lung cancer mortality reduction and deaths avoided. By estimating these key benefits at various screening adherence rates, we provide data that are necessary for health policy considerations and results that can serve as a tool to evaluate the impacts of existing screening programs. Our results assuming 100% adherence to lung cancer screening are presented in S3 Appendix and represent the maximum potential benefits and harms of a national lung cancer screening program.
Information on accessing US Census Bureau, NLST, and PLCO data, as well as additional information regarding the “smoking history generator,” used in this study can be found in S1 Text. We have also provided output data from the LCPM used in producing our results for this study in S1 Data.
Results
Outcomes in the absence of screening
Lung cancer cases were estimated to decrease 21.90% in the absence of screening to 141,114 (95% CI 140,934–141,294) annually in 2030 from 180,673 (95% CI 180,424–180,921) in 2016, resulting in cumulative lung cancer cases of 2,462,479 (95% CI 2,459,721–2,465,237) over the period. Former smokers made up an estimated 54.28% of these lung cancers, while current smokers made up 35.68%, and never smokers made up only 10.04%.
In the absence of screening, our model projected 1,777,144 (95% CI 1,775,138–1,779,151) cumulative lung cancer deaths between 2016 and 2030 for all birth cohorts in the US, with former, current, and never smokers totaling 952,578 (53.60% of total, 95% CI 950,983–954,173), 686,780 (38.65% of total, 95% CI 684,998–688,562), and 137,786 (7.75% of total, 95% CI 137,287–138,286) lung cancer deaths, respectively.
Outcomes with screening
Total screens
Under the CMS screening eligibility criteria, cumulative screens through 2030 were projected to be 63,857,158 (95% CI 63,815,984–63,898,332). Fig 1 shows the total number of current and former smokers screened annually (Fig 1). Annual screens were estimated to decrease to 3,076,347 (95% CI 3,073,877–3,078,817) screens in 2030 (1.43% of study population) from 5,297,959 (95% CI 5,295,212–5,300,706) screens in 2016 (2.80% of study population). Throughout the study period, the majority of these simulated screens were of current smokers (decreasing slightly to 59.28% in 2030 from 62.12% in 2016); former smokers made up the remainder of these screens (increasing to 40.72% in 2030 from 37.88% in 2016).
Fig. 1. Projected total number of current and former smokers screened, 2016–2030. 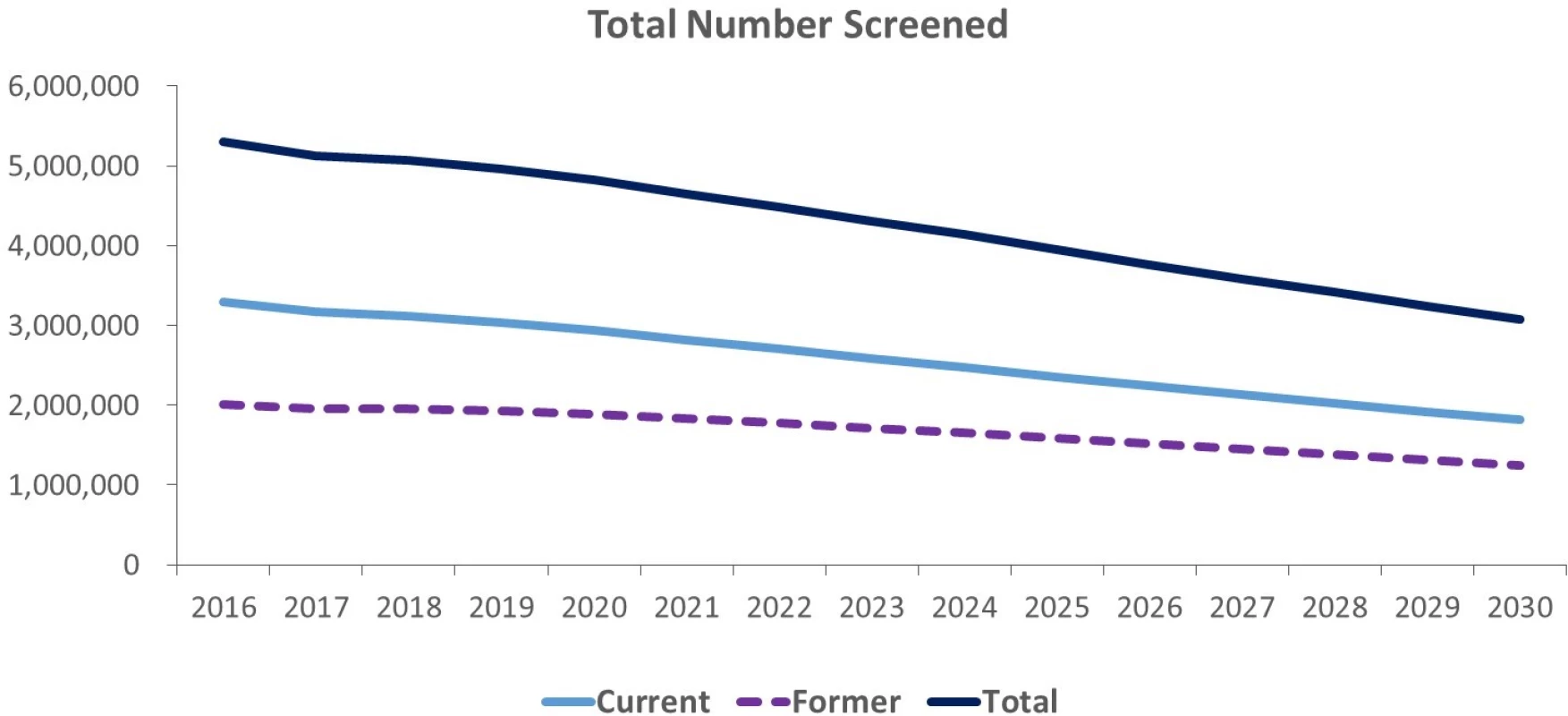
Screening with an assumed 45% adherence rate in 2016, our estimates showed that current smokers screened made up 4.36% of the overall simulated population between the screening-eligible ages of 55 and 77 years, while former smokers screened made up only 2.66% of the same population. By 2030, these estimated percentages had decreased considerably to 2.10% and 1.44% for current and former smoker screens (S2 Appendix), respectively. Projected total screens decreased by 41.93% over the period.
Mortality reduction
Mortality reduction is defined as the difference in lung cancer deaths between the no-screening and screening scenarios (i.e., deaths avoided), divided by the deaths in the no-screening scenario, giving the percentage of deaths in the no-screening scenario that could be avoided through screening. Cumulative lung cancer mortality reduction within the screened population (those individuals who were screened at least once) was estimated to be 16.98% (95% CI 16.90%–17.07%). Fig 2 compares lung cancer mortality reduction results from the NLST to those of the screened-only population, total population, and both smoker types in this study (Fig 2).
Fig. 2. Projected cumulative mortality reduction comparison to National Lung Screening Trial (NLST) results, 2016–2030. 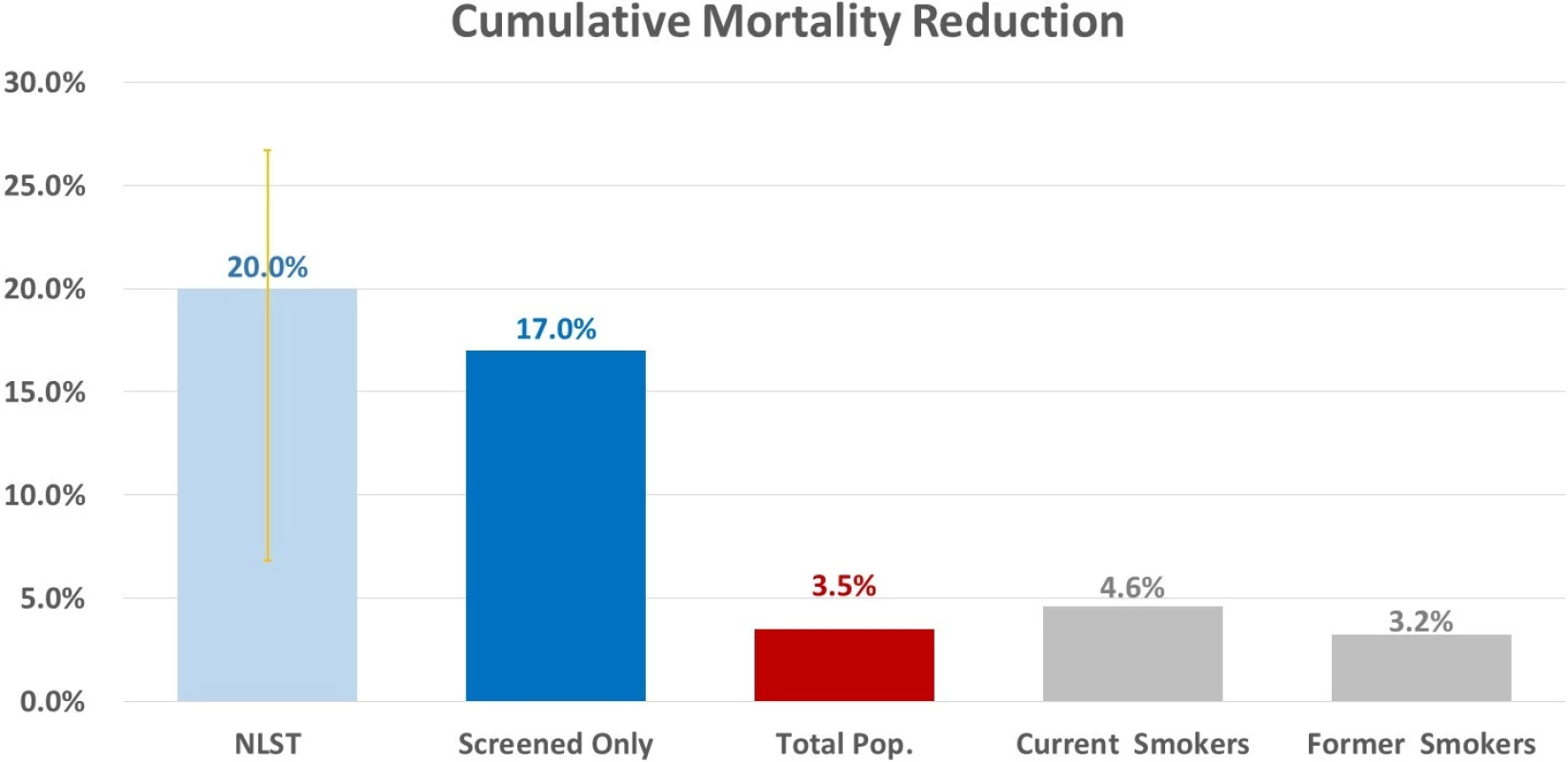
Pop., population. The total cumulative mortality reduction across the study population, inclusive of those ineligible for screening under the CMS guidelines and nonadherent individuals, was estimated to be 3.52% (95% CI 3.50%–3.53%) by 2030. Cumulative mortality reductions for current smokers and former smokers were estimated to be 4.58% (95% CI 4.54%–4.62%) and 3.25% (95% CI 3.22%–3.27%), respectively. Fig 3 shows cumulative mortality reduction stratified by smoker type and sex (Fig 3).
Fig. 3. Projected cumulative mortality reduction stratified by smoker type and sex, 2016–2030. 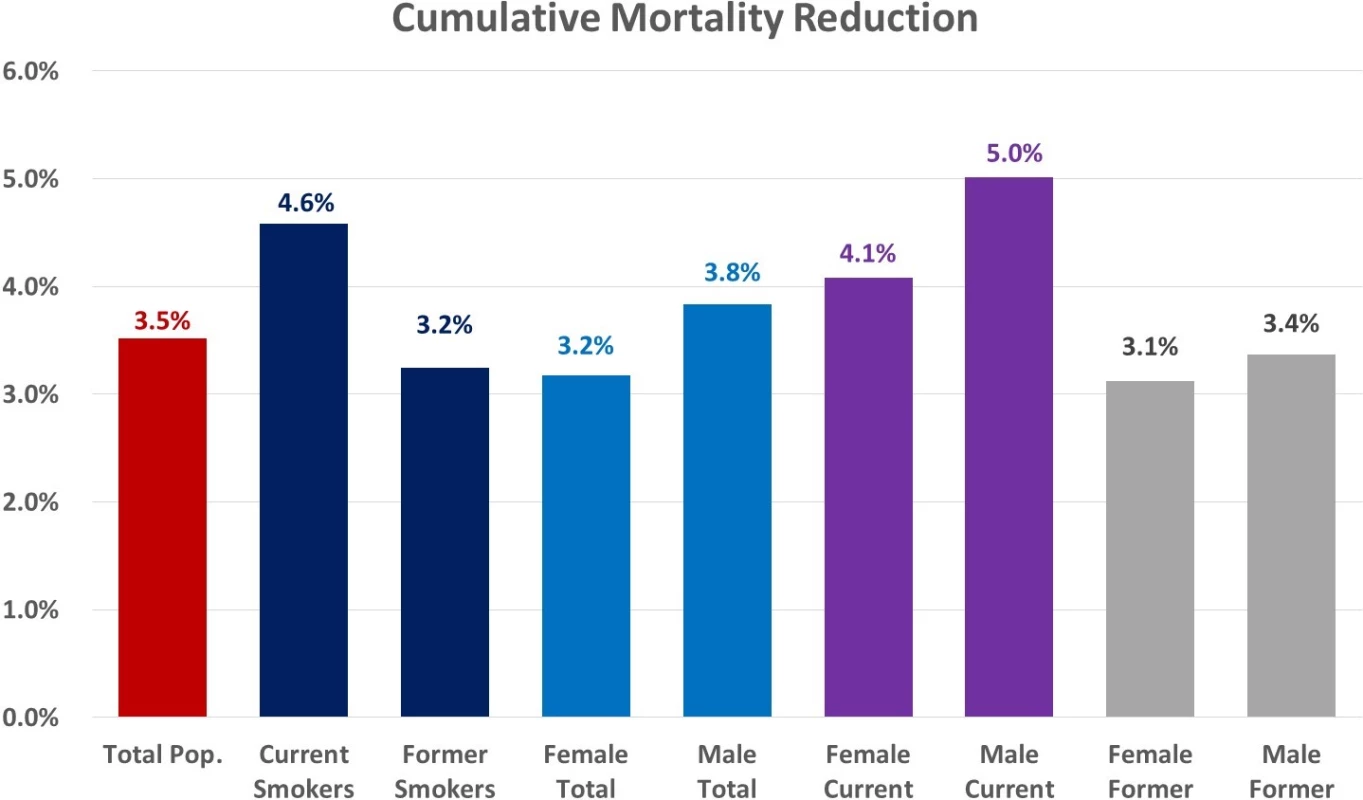
Pop., population. Projected annual mortality reduction for the study population peaked in 2021 at 4.38% (95% CI 4.36%–4.41%) and decreased to 3.53% (95% CI 3.50%–3.56%) by 2030 (Fig 4). Current smoker mortality reduction on an annual basis reached an estimated maximum of 5.69% (95% CI 5.65%–5.74%) in 2021 before decreasing to 4.76% (95% CI 4.70%–4.81%) by 2030, and former smoker mortality reduction reached an estimated maximum of 4.03% (95% CI 4.00%–4.07%) in 2022 before decreasing to 3.37% (95% CI 3.33%–3.41%) by 2030 (S2 Appendix).
Fig. 4. Projected mortality reduction for the total study population on an annual and a cumulative basis (extended past the study period to show trend). 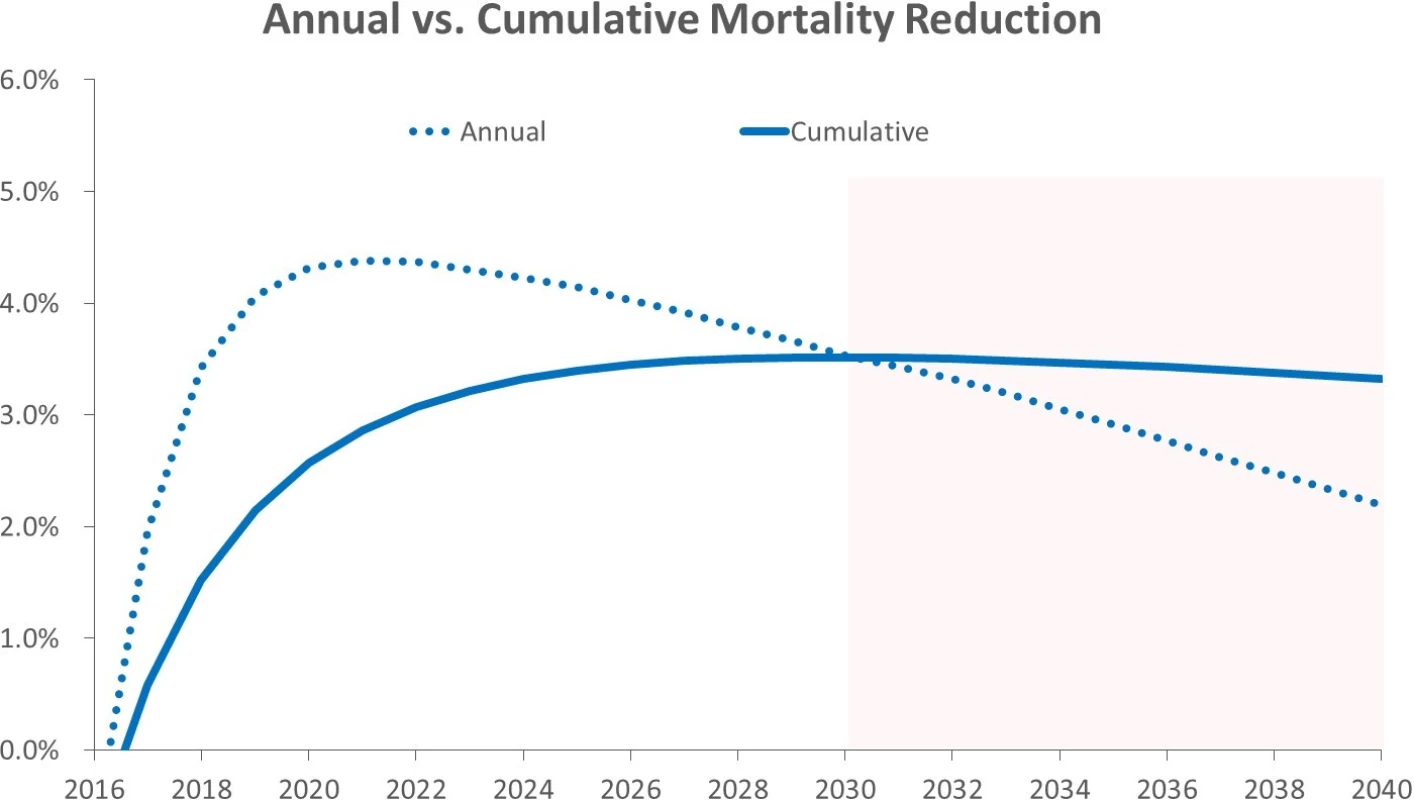
Estimated total deaths avoided amounted to 62,425 (95% CI 62,123–62,727), with current smokers accounting for 31,482 (95% CI 31,221–31,743) deaths avoided (50.43% of total) and former smokers accounting for 30,943 (95% CI 30,697–31,189) deaths avoided (49.57% of total) (Table 1). Our model predicted that the highest number of deaths could be avoided in the years 2021–2025, compared to the 5-year periods before and after.
Tab. 1. Estimated deaths avoided for current and former smokers compared to total population, 2016–2030. 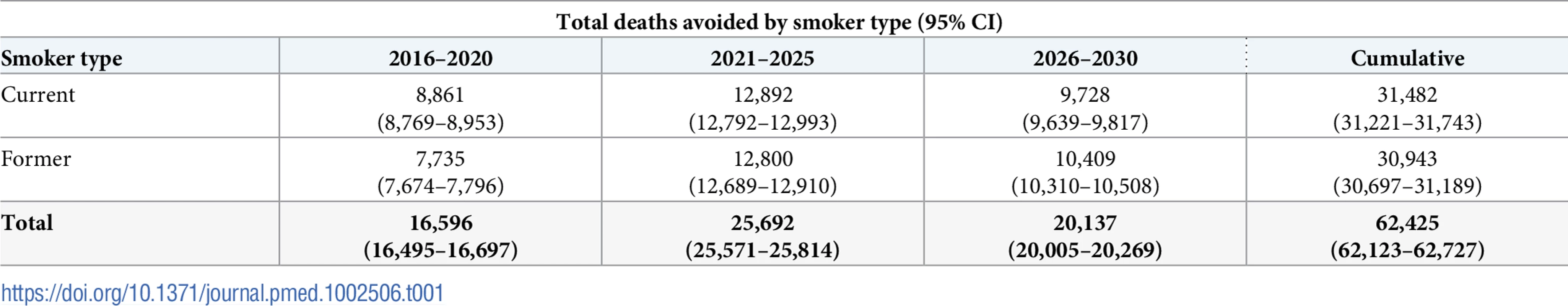
We estimated that the highest proportion of total deaths avoided occurred between ages 70–74 years, 75–79 years, and 65–69 years (29.52%, 29.39%, and 21.33% of total, respectively; S2 Appendix). These age ranges also had the highest shares of projected total lung cancer deaths in the absence of screening, with individuals aged 75–79 years, 70–74 years, and 65–69 years composing 23.01%, 22.40%, and 16.90% of the total, respectively.
Mortality reduction for individual birth cohorts
We estimated the mortality reduction for individual birth cohorts to demonstrate how the benefits of screening can vary between birth cohorts. Mortality reduction was assessed over a 15-year period, with the observation period, in some cases, extending past the 2030 end year employed elsewhere in this study. The 1960, 1970, and 1980 birth cohorts had estimated cumulative mortality reductions of 4.12% (95% CI 4.10%–4.14%), 2.74% (95% CI 2.72%–2.75%), and 1.97% (95% CI 1.97%–1.98%), respectively. Projected mortality reduction trended downward for more recent birth cohorts, reflecting the overall trend of decreasing smoking prevalence in the US (Fig 5, S2 Appendix).
Fig. 5. Projected cumulative mortality reduction for single birth cohorts. 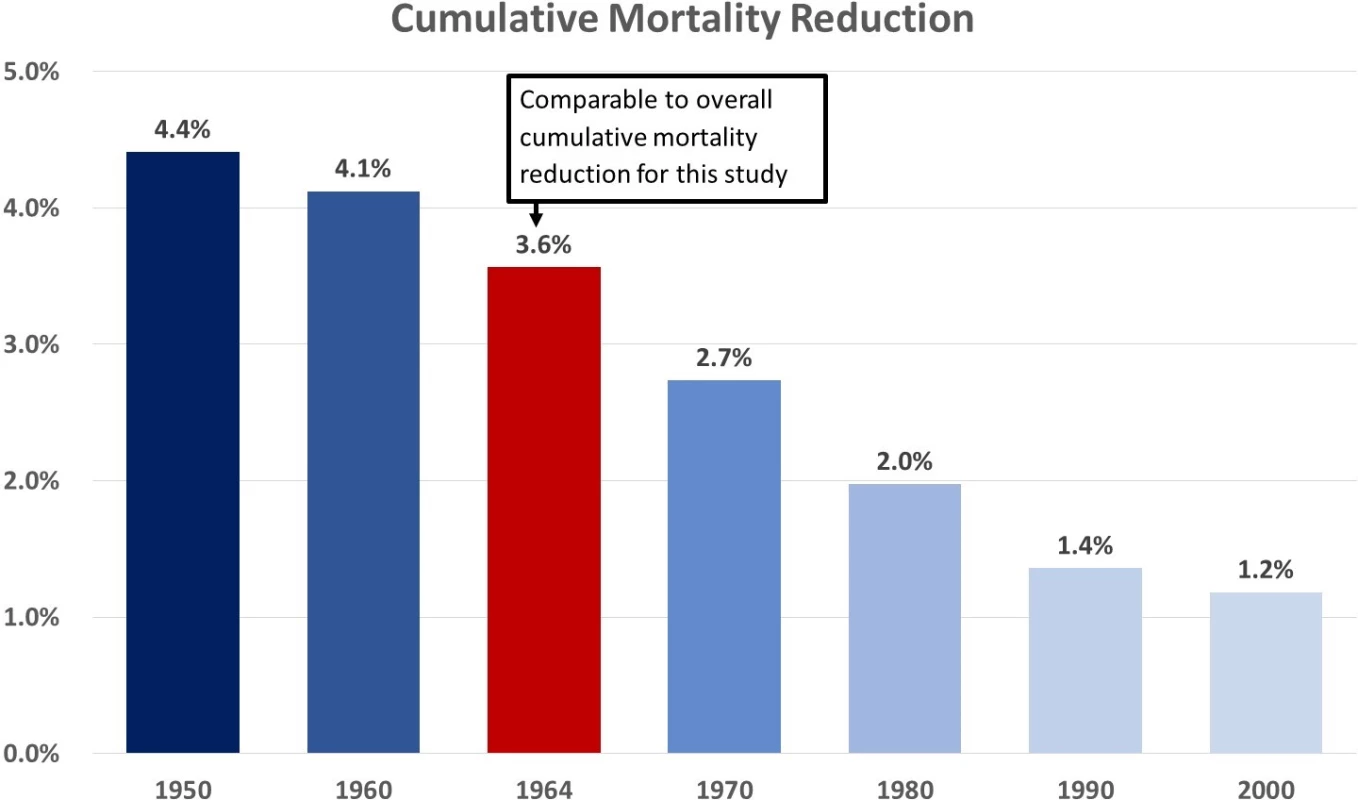
Life-years gained
Lung cancer screening with the CMS guidelines would save a projected 148,484 (95% CI 147,429–149,540) life-years across the total population through 2030. Simulated current smokers benefitted most in terms of life-years saved, with a total of 104,315 (95% CI 102,570–106,060), while simulated former smokers derived considerably less benefit in terms of life-years saved, with only 44,169 (95% CI 43,192–45,147) total.
Overdiagnoses
Overdiagnosed cases in this study are defined as those in which an individual is screened and subsequently diagnosed with lung cancer but eventually dies of causes other than lung cancer. These are deemed overdiagnoses because these additional lung cancer diagnoses that occur in the screening scenario compared to the no-screening scenario would have likely had limited negative consequences if they had remained undetected because of absence of screening [29].
Overdiagnosed cases were estimated to be 9,054 (95% CI 9,011–9,098), compared to an estimated 62,425 total deaths avoided via screening, yielding 14.50 overdiagnoses for every 100 deaths avoided. Compared to the 252,429 (95% CI 251,208–253,649) projected screen-detected lung cancer diagnoses, the estimated overdiagnosis rate was 3.59%. Patients aged 70–74 years made up the largest portion of these overdiagnoses with an estimated 3,417 (95% CI 3,400–3,433), while patients aged 75–79 years also made up a significant amount of the overdiagnoses with an estimated 3,196 (95% CI 3,181–3,212), together making up 73.04% of all projected overdiagnoses (S2 Appendix).
We also compared overdiagnoses in our study to those estimated in the NLST. Patz et al. previously developed an excess cancer diagnosis rate considering a public health perspective to estimate the true level of overdiagnosis in the NLST [29]. This definition takes the difference in the number of lung cancer cases between the low-dose CT screening arm and the chest X-ray (control) arm and divides this number by the total number of lung cancers diagnosed in the low-dose CT arm [29]. This calculation provides the percentage of lung cancer diagnoses in the low-dose CT arm that are in excess of those that would have been diagnosed through clinical presentation or other means without screening. Using this method with our no-screening scenario as the control and 100% adherence (given adherence in the NLST was nearly 100%), our overdiagnosis rate was estimated to be 9.46% (95% CI 9.42%–9.51%), comparable to the 11.0% result of the Patz study [29]. S2 Appendix provides a comparison of these 2 methods for different age ranges.
Impacts of screening adherence
Reported adherence rates vary between different studies and will likely have a considerable impact on the efficacy of screening. To quantify the potential impact of adherence, we estimated the cumulative lung cancer mortality reduction and deaths avoided for the total population with screening adherence rates of 25% to 75% and perfect adherence (100%), given the inconclusiveness of published data on the matter (Table 2). Mortality reduction in the perfect adherence scenario was estimated to be 7.81% (95% CI 7.77%–7.85%), and an estimated 138,722 (95% CI 138,052–139,393) deaths were avoided, representing a missed opportunity to avoid approximately 76,297 more lung cancer deaths if all eligible patients participated in screening, compared to the 45% adherence rate used in this study. If a national lung cancer screening program were able to attain an adherence rate of 75%, comparable to breast and cervical cancer screening (69.3% and 85.8%, respectively), our model predicted a mortality reduction of 5.86% (95% CI 5.83%–5.89%) and 104,042 (95% CI 103,539–104,545) deaths avoided.
Tab. 2. Sensitivity analysis for overall cumulative mortality reduction and total deaths avoided estimates by adherence rate. 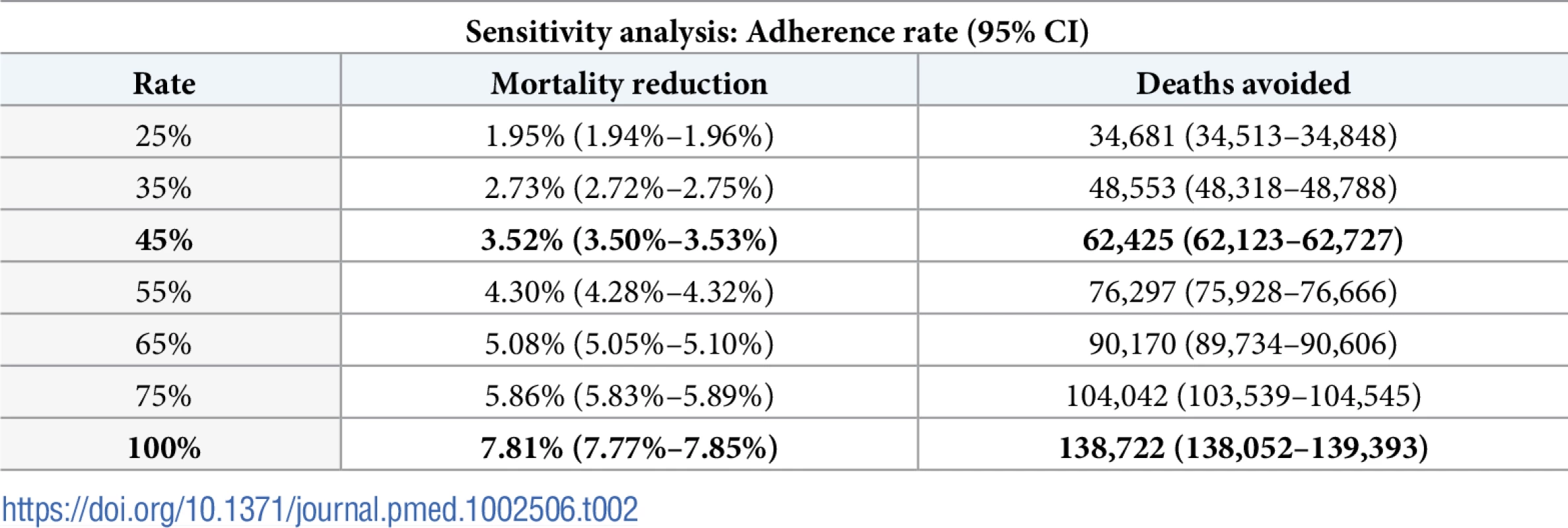
Discussion
Using the LCPM, we performed, to our knowledge, the first multiple birth cohort simulation study to estimate the health outcomes of lung cancer screening for the whole US population. Over the period 2016–2030, our model estimated that the number of people eligible for screening would decrease from 11,773,243 (95% CI 11,767,138–11,779,347) to 6,836,326 (95% CI 6,830,837–6,841,815). During this period, cumulative lung cancer mortality reduction was estimated to be 3.52% and 16.98% for the total population and screened individuals, respectively. The estimated lung cancer mortality reduction within the screened population was similar to the observed result of 20.0% in the NLST. Our study predicts that lung cancer screening at a population level would yield 14.50 overdiagnosed cases for every 100 deaths avoided and 3.59 overdiagnosed cases for every 100 cases of screen-detected lung cancer. We used a screening adherence rate of 45% in our base case scenario in order to provide realistic estimates of the benefit of a fully implemented lung cancer screening program. Compared to the results using an ideal adherence rate of 100%, the more practical rate used in our study demonstrates how improving the adherence rate is pivotal to the success of a population-level screening program.
Comparison to single birth cohort studies
Prior lung cancer screening modeling studies that followed a single birth cohort (e.g., a US cohort born in 1950) and used similar eligibility requirements and 100% adherence reported estimated mortality reduction to be approximately 14%—higher than our reported estimate of 7.81% for the US population with 100% adherence [10,11]. A potential mechanism for the difference in mortality reduction is the continuous turnover of eligible smokers in our multiple birth cohort analysis. Earlier birth cohorts with higher smoking prevalence (i.e., cohorts born in the 1950s and early 1960s) experience a higher lung cancer mortality reduction because there are more high-risk smokers eligible for screening and, thus, more opportunity for early detection of lung cancers. When single birth cohort analyses estimate lung cancer mortality reduction, they only capture the benefit at its maximum—with just 1 cohort that has considerably higher risk of lung cancer than do later cohorts. Therefore, the results of single birth cohort analyses are not generalizable to the US population as a whole.
In our study, simulated individuals from more recent birth cohorts with lower smoking prevalence are replacing these older smokers each year, resulting in a lower percentage of the study population eligible for screening. This can be seen by comparing the estimated 19% of the 1950 cohort eligible for screening in prior single cohort studies to the estimated 6.22% of our study population eligible in the first year of our analysis, when the most individuals from earlier cohorts are present [10,11]. The percentage eligible decreases to 3.17% over the study period, as more recent cohorts with lower smoking prevalence enter the study population.
Fewer eligible individuals translates into lower mortality reduction in later birth cohorts, as there are both fewer smokers being screened and fewer lung cancers to be detected. The results of our single birth cohort analyses provide a validation of this mechanism, showing higher estimated mortality reduction for earlier US cohorts (Fig 5, S2 Appendix). Our lower estimated mortality reduction is, therefore, a product of lower risk birth cohorts partially offsetting the higher benefit derived by earlier birth cohorts.
Studying multiple birth cohorts over an extended period of time captures changes in smoking prevalence and gives a practical view of the benefit of screening for public health policy decision making. Single cohort simulation studies can be more easily implemented, but they neglect smoking behavior trends over different generations by providing only the benefits and harms for 1 cohort. Smoking prevalence strongly influences lung cancer incidence cases and deaths [30,31], thereby highlighting the need for an evaluation of lung cancer screening that considers the proportion of current and former smokers in the total population over time, as in this study.
Limitations
Because our study is meant to be an analysis of the US population at large, there is no explicit modeling of race or socioeconomic status in our projections of the health outcomes of lung cancer screening. Significant variation exists in the smoking behaviors of different races and individuals of different socioeconomic status, which can influence lung cancer incidence rates and access to care within these populations [32–35]. Due to these factors, individuals in these populations may not receive proportionate benefit, and therefore, our results may not be generalizable to particular stratums within the US population. While projecting the effects of screening for these subpopulations would be valuable, the LCPM does not currently have the capability to model US smoking behavior at this level of detail (i.e., with stratifications by race and socioeconomic status). However, the development of a more comprehensive model to estimate screening effects for these subpopulations is currently the focus of ongoing research by the CISNET consortium.
An additional limitation of this study is that our model was calibrated to data from the NLST and PLCO [22]. These studies were performed in academic centers and may have enrolled healthier individuals in better-organized screening programs compared to the average community health center. Therefore, the conditions under which these studies were executed may not be representative of screening programs implemented at health centers across the country. These differences between academic trials and screening programs at the average community health center could translate to slightly lower overall effectiveness when considering a national screening program. The primary driver of this lower effectiveness would likely be reduced screening adherence due to lower quality healthcare infrastructure and more patients with serious comorbidities being unable to receive screening. These differences are taken into account in the 45% adherence rate used for this study and are further explored in the sensitivity analysis on screening adherence rate, though other differences in the quality of facilities, providers, and treatments could also impact effectiveness.
Finally, our study is limited in that it is confined to the guidelines issued by the CMS. We do not evaluate whether a better screening strategy for lung cancer mortality reduction exists in comparison to the CMS guidelines but rather estimate the national impact of the current guidelines issued by the CMS. In doing so, the eligible age in our study extends to 77 years, which could include individuals who are technically eligible based on smoking history and age but would not be screened because of comorbidities.
Implications
Although lower than the mortality reduction estimated by single cohort studies, our study’s projected mortality reduction demonstrates the potential efficacy of screening with low-dose CT for the many birth cohorts that constitute the US population if adherence rates are improved. Further demonstrating lung cancer screening’s value to the US population, screening was projected to save 148,484 life-years. The estimated harms—mainly overdiagnoses—associated with screening were minimal compared to these potential benefits. While overdiagnoses cause patients to endure unnecessary treatment, morbidity, cost, and potential anxiety, only in very rare cases do they cause death [29,36]. Therefore, the estimated benefits of lung cancer screening on a population level would likely outweigh these harms attributable to overdiagnosis.
With an estimated 138,722 deaths that could be avoided by 2030 with 100% adherence, lung cancer screening using the CMS guidelines provides an opportunity for substantial benefit to the US population yet remains challenged by the need for improving and maintaining adherence to screening. With the resources and guidelines available to implement a comprehensive screening program in the US, greater efforts must be made to reach high-risk smokers and make known the advantages and limited downsides of participating in screening. The projected impact of adherence on screening effectiveness shown in our study highlights this need for more comprehensive action to raise awareness and encourage adherence to guidelines [9,37,38].
While screening has been shown to reduce lung cancer mortality, decreasing smoking prevalence in more recent generations will eventually lower the effectiveness of a nationwide screening program. Our analysis of lung cancer screening at a population level illustrates the window of opportunity to secure significant benefit for those with lung cancer and when that window may close. Based on our projections, annual mortality reduction will peak in the next 5 years before declining because of lower smoking rates in younger birth cohorts. Therefore, the time frame for organizing and executing a strategy for nationwide lung cancer screening would ideally be in the coming years. Delays on fully implementing lung cancer screening will forfeit the opportunity to prevent more than 62,000 lung cancer deaths and minimize the burden of lung cancer in the next 15 years. As smoking prevalence declines, the effectiveness of a large-scale screening program, for the most part, becomes less favorable, and a change to the current policies regarding lung cancer control will be warranted.
While lung cancer screening is not seen by some as a health policy priority [39], the results demonstrated in this study should spur further conversation into how we can better use early detection to reduce the deadly consequences of lung cancer.
Supporting Information
Zdroje
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332 26742998.
2. Boer R, Moolgavkar SH, Levy DT. Chapter 15: Impact of tobacco control on lung cancer mortality in the United States over the period 1975-2000—summary and limitations. Risk Anal. 2012;32 Suppl 1:S190–201. doi: 10.1111/j.1539-6924.2012.01827.x 22882889; PubMed Central PMCID: PMC3430975.
3. Wender R, Fontham ET, Barrera E Jr., Colditz GA, Church TR, Ettinger DS, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63(2):107–17. doi: 10.3322/caac.21172 23315954; PubMed Central PMCID: PMC3632634.
4. International Early Lung Cancer Action Program I, Henschke CI, Yankelevitz DF, Libby DM, Pasmantier MW, Smith JP, et al. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med. 2006;355(17):1763–71. doi: 10.1056/NEJMoa060476 17065637.
5. Bach PB, Mirkin JN, Oliver TK, Azzoli CG, Berry DA, Brawley OW, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA. 2012;307(22):2418–29. doi: 10.1001/jama.2012.5521 22610500; PubMed Central PMCID: PMC3709596.
6. National Lung Screening Trial Research T, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873 21714641; PubMed Central PMCID: PMC4356534.
7. Moyer VA, Force USPST. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–8. doi: 10.7326/M13-2771 24378917.
8. Simard EP, Engels EA. Cancer as a cause of death among people with AIDS in the United States. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2010;51(8):957–62. Epub 2010/09/10. doi: 10.1086/656416 20825305; PubMed Central PMCID: PMC2943990.
9. Services CfMM. Decision memo for screening for lung cancer with low dose computed tomography. 2015. Available from: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274
10. McMahon PM, Meza R, Plevritis SK, Black WC, Tammemagi CM, Erdogan A, et al. Comparing benefits from many possible computed tomography lung cancer screening programs: extrapolating from the National Lung Screening Trial using comparative modeling. PLoS ONE. 2014;9(6):e99978. Epub 2014/07/01. doi: 10.1371/journal.pone.0099978 24979231; PubMed Central PMCID: PMC4076275.
11. de Koning HJ, Meza R, Plevritis SK, ten Haaf K, Munshi VN, Jeon J, et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160(5):311–20. doi: 10.7326/M13-2316 24379002; PubMed Central PMCID: PMC4116741.
12. Ten Haaf K, de Koning HJ. Overdiagnosis in lung cancer screening: why modelling is essential. J Epidemiol Community Health. 2015;69(11):1035–9. doi: 10.1136/jech-2014-204079 26071497; PubMed Central PMCID: PMC4978857.
13. Han SS, Ten Haaf K, Hazelton WD, Munshi VN, Jeon J, Erdogan SA, et al. The impact of overdiagnosis on the selection of efficient lung cancer screening strategies. Int J Cancer. 2017;140(11):2436–43. doi: 10.1002/ijc.30602 28073150; PubMed Central PMCID: PMC5516788.
14. Holford TR, Ebisu K, McKay L, Oh C, Zheng T. Chapter 12: Yale lung cancer model. Risk Anal. 2012;32 Suppl 1:S151–65. doi: 10.1111/j.1539-6924.2011.01754.x 22882886; PubMed Central PMCID: PMC3662537.
15. Holford TR, Clark L. Chapter 4: Development of the counterfactual smoking histories used to assess the effects of tobacco control. Risk Anal. 2012;32 Suppl 1:S39–50. doi: 10.1111/j.1539-6924.2011.01759.x 22882891; PubMed Central PMCID: PMC3490210.
16. Holford TR, Meza R, Warner KE, Meernik C, Jeon J, Moolgavkar SH, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964–2012. JAMA. 2014;311(2):164–71. doi: 10.1001/jama.2013.285112 24399555; PubMed Central PMCID: PMC4056770.
17. Holford TR, Levy DT, McKay LA, Clarke L, Racine B, Meza R, et al. Patterns of birth cohort-specific smoking histories, 1965–2009. Am J Prev Med. 2014;46(2):e31–7. doi: 10.1016/j.amepre.2013.10.022 24439359; PubMed Central PMCID: PMC3951759.
18. McMahon PM, Kong CY, Johnson BE, Weinstein MC, Weeks JC, Kuntz KM, et al. Estimating long-term effectiveness of lung cancer screening in the Mayo CT screening study. Radiology. 2008;248(1):278–87. Epub 2008/05/07. doi: 2481071446 [pii] doi: 10.1148/radiol.2481071446 18458247.
19. McMahon PM, Kong CY, Johnson BE, Weinstein MC, Weeks JC, Tramontano AC, et al. Chapter 9: The MGH-HMS lung cancer policy model: tobacco control versus screening. Risk Anal. 2012;32 Suppl 1:S117–24. Epub 2012/08/29. doi: 10.1111/j.1539-6924.2011.01652.x 22882882; PubMed Central PMCID: PMC3478757.
20. McMahon PM, Kong CY, Weinstein MC, Tramontano AC, Cipriano LE, Johnson BE, et al. Adopting helical CT screening for lung cancer: potential health consequences during a 15-year period. Cancer. 2008;113(12):3440–9. doi: 10.1002/cncr.23962 18988293; PubMed Central PMCID: PMC2782879. NIHMSID: NIHMS74571.
21. McMahon PM, Kong CY, Johnson BE, Weinstein MC, Weeks JC, Kuntz KM, et al. Estimating long-term effectiveness of lung cancer screening in the Mayo CT screening study. Radiology 2008;248(1):278–87. PubMed Central PMCID: PMCAccepted for publication Jan. 30, 2008; not subject to the NIH Public Access Policy. doi: 10.1148/radiol.2481071446 18458247
22. Meza R, ten Haaf K, Kong CY, Erdogan A, Black WC, Tammemagi MC, et al. Comparative analysis of 5 lung cancer natural history and screening models that reproduce outcomes of the NLST and PLCO trials. Cancer. 2014;120(11):1713–24. doi: 10.1002/cncr.28623 24577803; PubMed Central PMCID: PMC4031303.
23. Population Projections [Internet]. United States Census Bureau. 2017. Available from: https://www.census.gov/programs-surveys/popproj.html
24. Jeon J, Meza R, Krapcho M, Clarke LD, Byrne J, Levy DT. Chapter 5: Actual and counterfactual smoking prevalence rates in the U.S. population via microsimulation. Risk Anal. 2012;32 Suppl 1:S51–68. doi: 10.1111/j.1539-6924.2011.01775.x 22882892; PubMed Central PMCID: PMC3478148.
25. Kinsinger LS, Anderson C, Kim J, Larson M, Chan SH, King HA, et al. Implementation of Lung Cancer Screening in the Veterans Health Administration. JAMA Intern Med. 2017;177(3):399–406. doi: 10.1001/jamainternmed.2016.9022 28135352.
26. Lam VK, Miller M, Dowling L, Singhal S, Young RP, Cabebe EC. Community low-dose CT lung cancer screening: a prospective cohort study. Lung. 2015;193(1):135–9. doi: 10.1007/s00408-014-9671-9 25503535.
27. Duong DK, Shariff-Marco S, Cheng I, Naemi H, Moy LM, Haile R, et al. Patient and primary care provider attitudes and adherence towards lung cancer screening at an academic medical center. Prev Med Rep. 2017;6 : 17–22. doi: 10.1016/j.pmedr.2017.01.012 28210538; PubMed Central PMCID: PMC5304233.
28. Clarke TC, Soler-Vila H, Fleming LE, Christ SL, Lee DJ, Arheart KL. Trends in Adherence to Recommended Cancer Screening: The US Population and Working Cancer Survivors. Front Oncol. 2012;2 : 190. doi: 10.3389/fonc.2012.00190 23293767; PubMed Central PMCID: PMC3530735.
29. Patz EF Jr., Pinsky P, Gatsonis C, Sicks JD, Kramer BS, Tammemagi MC, et al. Overdiagnosis in low-dose computed tomography screening for lung cancer. JAMA internal medicine. 2014;174(2):269–74. doi: 10.1001/jamainternmed.2013.12738 24322569; PubMed Central PMCID: PMC4040004.
30. Tramontano AC, Sheehan DF, McMahon PM, Dowling EC, Holford TR, Ryczak K, et al. Evaluating the impacts of screening and smoking cessation programmes on lung cancer in a high-burden region of the USA: a simulation modelling study. BMJ open. 2016;6(2):e010227. Epub 2016/03/02. doi: 10.1136/bmjopen-2015-010227 26928026; PubMed Central PMCID: PMC4780060.
31. Moolgavkar SH, Holford TR, Levy DT, Kong CY, Foy M, Clarke L, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975–2000. J Natl Cancer Inst. 2012;104(7):541–8. doi: 10.1093/jnci/djs136 22423009; PubMed Central PMCID: PMC3317881.
32. Meza R, Meernik C, Jeon J, Cote ML. Lung cancer incidence trends by gender, race and histology in the United States, 1973–2010. PLoS ONE. 2015;10(3):e0121323. doi: 10.1371/journal.pone.0121323 25822850; PubMed Central PMCID: PMC4379166.
33. Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20(4):417–35. doi: 10.1007/s10552-008-9256-0 19002764; PubMed Central PMCID: PMC2711979.
34. Patel MI, Wang A, Kapphahn K, Desai M, Chlebowski RT, Simon MS, et al. Racial and Ethnic Variations in Lung Cancer Incidence and Mortality: Results From the Women's Health Initiative. J Clin Oncol. 2016;34(4):360–8. doi: 10.1200/JCO.2015.63.5789 26700122; PubMed Central PMCID: PMC4872034.
35. Underwood JM, Townsend JS, Tai E, Davis SP, Stewart SL, White A, et al. Racial and regional disparities in lung cancer incidence. Cancer. 2012;118(7):1910–8. doi: 10.1002/cncr.26479 21918961.
36. Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005. doi: 10.1056/NEJMoa1206809 23171096.
37. Detterbeck FC, Mazzone PJ, Naidich DP, Bach PB. Screening for lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e78S–e92S. doi: 10.1378/chest.12-2350 23649455; PubMed Central PMCID: PMC3749713.
38. Marshall HM, Bowman RV, Yang IA, Fong KM, Berg CD. Screening for lung cancer with low-dose computed tomography: a review of current status. J Thorac Dis. 2013;5 Suppl 5:S524–39. doi: 10.3978/j.issn.2072-1439.2013.09.06 24163745; PubMed Central PMCID: PMC3804881.
39. Piana R. The Ongoing Challenges of Lung Cancer Screening. The ASCO Post. 2017 May 25, 2017.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2018 Číslo 2- Berberin: přírodní hypolipidemikum se slibnými výsledky
- Příznivý vliv Armolipidu Plus na hladinu cholesterolu a zánětlivé parametry u pacientů s chronickým subklinickým zánětem
- Hydrofilní gel na bázi medu v terapii chronických a infikovaných ran
- Jakým mýtům o štítné žláze věří naši pacienti?
- Superoxidovaný roztok a jeho využití v léčbě ran
-
Všechny články tohoto čísla
- Setbacks in Alzheimer research demand new strategies, not surrender
- Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial
- Susceptibility of to azithromycin and ceftriaxone in China: A retrospective study of national surveillance data from 2013 to 2016
- Population impact of lung cancer screening in the United States: Projections from a microsimulation model
- Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site
- The potential impact of case-area targeted interventions in response to cholera outbreaks: A modeling study
- Perfluoroalkyl substances and changes in body weight and resting metabolic rate in response to weight-loss diets: A prospective study
- The 2014–2015 Ebola virus disease outbreak and primary healthcare delivery in Liberia: Time-series analyses for 2010–2016
- Prevalence of sexually transmitted infections and bacterial vaginosis among women in sub-Saharan Africa: An individual participant data meta-analysis of 18 HIV prevention studies
- Preventing cholera outbreaks through early targeted interventions
- Diet during pregnancy and infancy and risk of allergic or autoimmune disease: A systematic review and meta-analysis
- Risk and surrogate benefit for pediatric Phase I trials in oncology: A systematic review with meta-analysis
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- The potential impact of case-area targeted interventions in response to cholera outbreaks: A modeling study
- Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site
- Susceptibility of to azithromycin and ceftriaxone in China: A retrospective study of national surveillance data from 2013 to 2016
- Perfluoroalkyl substances and changes in body weight and resting metabolic rate in response to weight-loss diets: A prospective study
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



