-
Články
Reklama
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
ReklamaNovel Strategies to Enhance Vaccine Immunity against Coccidioidomycosis
article has not abstract
Published in the journal: . PLoS Pathog 9(12): e32767. doi:10.1371/journal.ppat.1003768
Category: Pearls
doi: https://doi.org/10.1371/journal.ppat.1003768Summary
article has not abstract
A Primary Pathogen of Mammalian Hosts
Coccidioidomycosis is a potentially life-threatening respiratory mycosis endemic to the Americas and caused by inhalation of spores produced by the molds Coccidioides immitis and C. posadasii. The dry, air-dispersed infectious spores (arthroconidia) are derived from saprobic-phase filaments that grow in semidesert soil of the southwestern United States and arid regions of Mexico and Central and South America [1]. Coccidioides is a dimorphic ascomycetous fungus with distinct saprobic and parasitic phases and is classified in the order Onygenales together with other genera of pathogenic molds that include Histoplasma, Blastomyces, and Paracoccidioides. The clinical spectrum of disease caused by these environmental pathogens ranges from a mild infection that resolves spontaneously to a disseminated mycosis. Inhaled spores of Coccidioides are small enough to colonize the lowermost reaches of the respiratory tree. Nonhuman primates experimentally challenged by aerosolization with fewer than ten infectious propagules developed a severe form of the disease and died within four to six weeks [2]. The parasitic cycle of Coccidioides is unique among these medically important, dimorphic molds. Spores in the lungs germinate to form multinucleate spherules (>60 µm diameter) that are too large to be engulfed by host phagocytes. The contents of mature spherules differentiate into a multitude of propagative endospores. Production of indigestible spherules that display high fecundity during the endosporulation stage confound phagocytic defenses and augment survival of the fungus in the lungs. Mammalian innate immune defenses are further compromised by the ability of endosporulating spherules to generate an alkaline microenvironment at infection sites due to their release of ammonia, which contributes to the pathogen's virulence [3].
Need for a Vaccine
The incidence of symptomatic coccidioidomycosis in the United States increased from 2,265 reported cases in 1998 to 22,401 in 2011 based on data from the National Notifiable Diseases Surveillance System (NNDSS) [4]. This database likely underestimates the actual burden of disease. Reporting cases of Valley Fever is not mandated in every state within known areas of endemicity. Moreover, Coccidioides has established niches in nontraditional endemic regions not considered in the report [5]. Approximately 10% of the total United States population resides in the Southwest, including more than 300 thousand military personnel who train in the semidesert terrain. Racial heritage (e.g., African and Filipino) influences susceptibility to this mycosis, although the immunologic mechanism is unclear [6]. Millions of tourists also visit popular landmarks in Texas, Arizona, and southern California, and although many people are exposed to Coccidioides spores, the majority (>60%) do not develop symptomatic disease. Nevertheless, a significant number of these individuals are diagnosed with reactivated infection months to years after returning home. Risk of infection is particularly high during dust storms, which occur in the spring and summer in endemic regions (http://directorsblog.health.azdhs.gov/?tag=valley-fever). A vaccine against coccidioidomycosis would arguably promote the well-being of at-risk populations in the United States in addition to people who reside in arid areas of Latin America. A compelling argument for the feasibility of such a vaccine is based on retrospective clinical evidence that individuals who recover from symptomatic coccidioidal infection remain skin-test positive and likely acquire life-long immunity to the disease. Both clinical data and results of experimental animal studies have shown that T-cell immunity is essential for protection against coccidioidomycosis and mammalian hosts with deficiency of CD4+ T cells are at elevated risk of contracting the respiratory disease [7]. A vaccine development strategy must, therefore, be designed to protect immunocompetent and as well as immunocompromised individuals. A formalin-killed spherule vaccine was tested in a clinical trial between 1980 and 1985 and, although there was a trend toward reduced disease, reactogenicity at sites of immunization was too great, requiring the vaccine dose to be reduced and thus underpowered [8]. Nevertheless, this early pioneering study laid the foundation for current efforts to generate a human vaccine.
A Novel Adjuvant Enhances Cellular Immunity Induced by a Live Vaccine
For many diseases in which natural infection confers protective immunity against reinfection, live vaccines have been successful in promoting robust and durable immune defenses in humans. An attenuated mutant of Coccidioides was generated by disruption of two chitinase genes that resulted in the inability of the organism to endosporulate [9]. Inbred mice immunized subcutaneously with the attenuated strain all survived after intranasal challenge with a potentially lethal spore inoculum. However, sterile immunity was not achieved and pulmonary tissue damage associated with a persistent host inflammatory response was evident, especially in BALB/c mice. Neutrophil migration to infected lungs plays a pivotal role during the early protective response [10], but persistence of these innate immune cells in the presence of elevated inflammatory cytokines IL-1β, IL-1α, and TNF-α leads to acute lung injury and disease exacerbation. BALB/c and C57BL/6 mouse strains differ in their ability to regulate inflammation associated with coccidioidal lung infection, possibly simulating a clinical difference that partly accounts for the heterogeneity of human immune responses to coccidioidomycosis. Infected BALB/c mice that had been immunized with the live, attenuated vaccine consistently revealed 8-fold higher numbers of lung-infiltrated neutrophils and significantly increased fungal burden compared to vaccinated C57BL/6 mice [9], [11], [12]. Thus, excessive inflammation due to persistent high neutrophil counts appears to compromise vaccine immunity.
We speculated that if the protracted recruitment of neutrophils to infection sites could be downregulated in BALB/c mice, the outcome could be improved. We accomplished this using a novel adjuvant conjugated with the live Coccidioides vaccine. A decapeptide agonist of the biologically active C-terminal region of human complement component C5a functions as an adjuvant that enhances antigen processing by antigen presenting cells (APCs) and promotes cellular immunity. Unique conformational features of this agonist allow it to bind with high affinity to C5a receptors (C5aR/CD88) on macrophages (MΦ) and dendritic cells (DC) but not neutrophils [13]. The adjuvant, termed EP67, was conjugated with lysine residues on the surface of live arthroconidia from the vaccine strain [14] (Figure 1A). Spore hydration and dilation steps physically fractured the cysteine-rich, hydrophobic outer wall, permitting EP67 conjugation with underlying cell wall components. EP67 directs the vaccine to C5aR-bearing MΦ and DC, inducing phagocytosis and antigen presentation. BALB/c mice immunized with the EP67-conjugated, live vaccine revealed increased survival, reduction of inflammatory pathology, lower fungal burden, and decreased recruitment of neutrophils to the lungs at 11 days post-challenge compared to mice immunized with the nonconjugated vaccine. The EP67 adjuvant enhanced vaccine protection by augmenting T-cell immunity, especially T-helper 1 (Th1) and Th17 responses [12]. Th17 immunity is indispensable for protection against coccidioidomycosis [11]. Although not yet approved for use in humans, EP67 is a promising adjuvant that drives relevant pathways of protective immunity to Coccidioides infection. However, in spite of these positive results, live vaccines are not ideal for immunocompromised individuals at risk of severe reaction to the attenuated strain, which highlights the need for safer and more efficacious vaccines using purified antigens, appropriate adjuvants, and efficient antigen delivery systems.
Fig. 1. Novel adjuvant and vaccine delivery system for enhancement of protective immunity to coccidioidomycosis. (A) An agonist of human complement fragment C5a (EP67) bound to live cells of an attenuated vaccine strain of Coccidioides enhances T-cell immunity while downregulating inflammatory pathology. 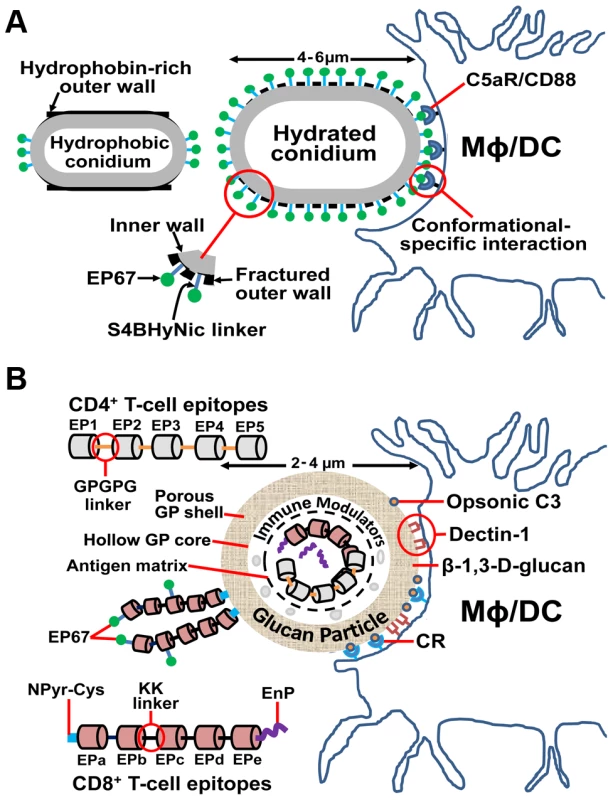
Hydration and dilation of live arthroconidia of the vaccine strain results in fracture of the hydrophobic outer conidial wall and exposure of lysine residues of the underlying inner wall that can conjugate with EP67 via S4BHyNic linkers (succinimidyl-4-benzoylhydrazino-nicotinamide). The concept is that the engineered conformational features of EP67 direct the conjugated vaccine to C5aR/CD88 receptors on DC and MΦ, but not neutrophils, and activate phagocytosis, antigen processing, and presentation by APCs while dampening persistent neutrophil-associated inflammation at infection sites [12], [13]. (B) A glucan particle (GP)-based subunit vaccine platform combines adjuvanicity with antigen delivery to induce robust and durable CD4+ and CD8+ T-cell responses to Coccidioides infection. GPs are composed of a porous shell and hollow core. The protein vaccine is co-loaded with a carrier protein and interacted with yeast RNA within the core to form an antigen complex that is too large to diffuse out through the shell. Endo-Porter (EnP) peptides added to the antigen matrix enhance release of the CD8+ vaccine proteins to the cytoplasm of APCs after phagocytosis of GPs and promote processing and presentation of MHC I complexes, resulting in activation of protective CD8+ T cells. Between the antigen matrix and shell is a GP layer that can accommodate immune modulators (e.g., CpG, siRNA) that help to elicit a protective response to infection. Multiepitope constructs also may be coupled to the surface of GPs by addition of a pyridyl-S-cysteine peptide at the N-terminus (NPyr-Cys) of the vaccine protein. The C-terminus of GP surface-coupled vaccine proteins may be conjugated with EP67 as in Figure 1A. EP67 directs the EBV to complement receptors and, although not yet tested, may further enhance Th17 immunity. CD4+ and CD8+ multiepitope vaccines are constructed using nonimmunogenic GPGPG or di-lysine (KK) linkers [25], [26]. β-1,3-glucans and opsonic C3 deposited on the surface of GPs bind to Dectin-1 and complement receptors (CR), respectively, and induce phagocytosis by APCs (MΦ and DC) followed by antigen processing and peptide epitope display as MHC I or II complexes [17], [19]. An Innovative Adjuvant and Delivery Platform Contributes to the Protective Efficacy of Alternative Subunit Vaccines
Although CD4+ T cells are central to the mammalian protective response to Coccidioides infection, CD8+ T cells also mediate vaccine immunity [15]. Recent studies of infections caused by other dimorphic fungal pathogens have revealed that even in the absence of CD4+ T-cell help vaccine-induced IL-17–producing CD8+ T cells (Tc17) show long-term survival and confer protection [16]. This plasticity of cellular immunity argues for the feasibility of developing a vaccine against coccidioidomycosis in patients with immune deficiencies, including those with few or no CD4+ T cells. Our strategy in the design of a subunit vaccine has been to generate polypeptide constructs containing multiple immunodominant CD4+ or CD8+ T-cell epitopes that bind promiscuously to human major histocompatibility complex class II (MHC II) and MHC I molecules, respectively. T-cell epitopes were initially predicted by immunoinformatic sequence analysis of a selection of the many antigenic proteins of Coccidioides shown to induce protection against coccidioidal lung infections in mice [17]. Immunoreactivity of synthetic epitope peptides was validated by human MHC-specific binding assays and stimulation of immune T-cells in vitro to produce protective Th1 and Th17 cytokines. Epitope-based vaccines (EBV) against microbial diseases have been shown to be immunologically potent, relatively easy to produce, and are predicted to be safe in humans [18]. Bacterial-expressed recombinant CD4+ and CD8+ T-cell epitopes joined by nonimmunogenic linkers have been loaded into glucan particles (GPs), which deliver the EBV to APCs and serve as a potent adjuvant system [19] (Figure 1B). The selected epitopes are conserved between C. immitis and C. posadasii [17]. GPs are purified, hollow, porous shells made by alkali and acid extraction of baker's yeast, composed primarily of β-1,3-glucans, and essentially devoid of proteins, lipids, and mannans. GPs activate the alternative pathway of complement, leading to deposition of C3 fragments. GPs are phagocytosed by MΦ and DC via complement receptors and Dectin-1. Epitope-based vaccines composed of CD4+ or CD8+ epitopes can either be loaded into GPs or conjugated to the GP surface. EP67 conjugation with epitope-based protein vaccines may provide an effective mechanism to further augment Th17 immunity. CD8+ epitope–based vaccines internalized by DC and presented as peptide-MHC class I complexes can be enhanced by binding the EBV to a weak-base amphiphilic peptide (Endo-Porter) that promotes antigen release into the cytoplasm of APCs [20]. The GP core can accommodate various adjuvant classes to fine-tune immune responses and generate optimal and durable protection. The core of the loaded GP forms a central antigen matrix with a surrounding layer that accommodates immune modulators. For example, an oligodeoxynucleotide adjuvant (CpG) loaded into a GP-internalized, CD4+ epitope preparation and used to immunize mice against intranasal infection significantly improved protection compared to the same vaccine admixed with CpG in the absence of GPs [17]. Further, Endo-Porter has been shown to form stable nanocomplexes with small interfering RNAs (siRNAs), which when loaded into GPs and delivered to phagocytic cells can downregulate proinflammatory signaling and curb inflammatory pathology [21]. The glucan particle delivery and adjuvant platform offers multiple options for application of molecular tools that can optimally tailor a human epitope-based vaccine against coccidioidomycosis. Corporate partners currently evaluating the GP delivery technology are planning to carry out prerequisite toxicology and safety studies prior to the submission of an application for human testing.
Future Directions
Development of an effective coccidioidomycosis vaccine faces several major challenges. Reported studies to date have assumed that eliciting cell-mediated immunity will translate to protection against the disease. However, the role of humoral response to infection is still largely unexplored. It may be possible to protect inbred mice with a vaccine that elicits cell-mediated immunity alone, but we cannot assume that this observation will translate to humans. A recent vector-based vaccine against tuberculosis intended to protect by eliciting strong CMI failed in humans despite showing efficacy in mice [22]. Most cases of coccidioidomycosis recorded in the United States occur in individuals over 60 years of age [4]. Vaccine development for the elderly must take into account the aging immune system, a condition that may increase vulnerability to infectious diseases [23]. A coccidioidomycosis vaccine potentiated by an adjuvant specifically designed to stimulate the immune system of this demographic group (e.g., EP67) [24] is a current research priority.
Zdroje
1. FisherFS, BultmanMW, JohnsonSM, PappagianisD, ZaborskyE (2007) Coccidioides niches and habitat parameters in the southwestern United States: a matter of scale. Ann N Y Acad Sci 1111 : 47–72.
2. BlundellGP, CastleberryMW, LoweEP, ConverseJL (1961) The pathology of Coccidioides immitis in the Macaca mulatta. Am J Pathol 39 : 613–630.
3. WiseHZ, HungCY, WhistonE, TaylorJW, ColeGT (2013) Extracellular ammonia at sites of pulmonary infection with Coccidioides posadasii contributes to severity of the respiratory disease. Microb Pathog 59–60 : 19–28.
4. Anonymous (2013) Increase in reported coccidioidomycosis - United States, 1998–2011. Morb Mortal Wkly Rep 62 : 217–221.
5. Marsden-HaugN, GoldoftM, RalstonC, LimayeAP, ChuaJ, et al. (2013) Coccidioidomycosis acquired in Washington State. Clin Infect Dis 56 : 847–850.
6. RuddyBE, MayerAP, KOMG, LabonteHR, BorovanskyJA, et al. (2011) Coccidioidomycosis in African Americans. Mayo Clin Proc 86 : 63–69.
7. ColeGT, HurtgenBJ, HungC-Y (2012) Progress toward a human vaccine against coccidioidomycosis. Curr Fungal Infect Rep 6 : 235–244.
8. PappagianisD (1993) Evaluation of the protective efficacy of the killed Coccidioides immitis spherule vaccine in humans. The Valley Fever Study Group. Am Rev Respir Dis 148 : 656–660.
9. XueJ, ChenX, SelbyD, Hung-Y, YuJ-J, ColeGT (2009) A genetically engineered live attenuated vaccine of Coccidioides posadasii protects BALB/c mice against coccidioidomycosis. Infect Immun 77 : 3196–3208.
10. BalamayooranT, BatraS, BalamayooranG, CaiS, KobayashiKS, et al. (2011) Receptor-interacting protein 2 controls pulmonary host defense to Escherichia coli infection via the regulation of interleukin-17A. Infect Immun 79 : 4588–4599.
11. HungC-Y, GonzalezA, WüthrichM, KleinBS, ColeGT (2011) Vaccine immunity to coccidioidomycosis occurs by early activation of three signal pathways of T helper cell response (Th1, Th2, and Th17). Infect Immun 79 : 4511–4522.
12. HungC-Y, HurtgenBJ, BellecourtM, SandersonSD, MorganEL, et al. (2012) An agonist of human complement fragment C5a enhances vaccine immunity against Coccidioides infection. Vaccine 30 : 4681–4690.
13. MorganEL, MorganBN, SteinEA, VitrsEL, ThomanML, et al. (2009) Enhancement of in vivo and in vitro immune functions by a conformationally biased, response-selective agonist of human C5a: implications for a novel adjuvant in vaccine design. Vaccine 28 : 463–469.
14. PhillipsJA, MorganEL, DongY, ColeGT, McMahanC, et al. (2009) Single-step conjugation of bioactive peptides to proteins via a self-contained succinimidyl bis-arylhydrazone. Bioconjug Chem 20 : 1950–1957.
15. FiererJ, WatersC, WallsL (2006) Both CD4+ and CD8+ T cells can mediate vaccine-induced protection against Coccidioides immitis infection in mice. J Infect Dis 193 : 1323–1331.
16. NanjappaSG, HeningerE, WüthrichM, GasperDJ, KleinBS (2012) Tc17 cells mediate vaccine immunity against lethal fungal pneumonia in immune deficient hosts lacking CD4+ T cells. PLoS Pathog 8: e1002771 doi:10.1371/journal.ppat.1002771
17. HurtgenBJ, HungC-Y, OstroffGR, LevitzSM, ColeGT (2012) Construction and evaluation of a novel recombinant T cell epitope-based vaccine against coccidioidomycosis. Infect Immun 80 : 3960–3974.
18. RosaDS, RibeiroSP, Cunha-NetoE (2010) CD4+ T cell epitope discovery and rational vaccine design. Arch Immunol Ther Exp (Warsz) 58 : 121–130.
19. HuangH, OstroffGR, LeeCK, SpechtCA, LevitzSM (2010) Robust stimulation of humoral and cellular immune responses following vaccination with antigen-loaded β-glucan particles. MBio 1: e00164–10.
20. IkeuchiN, FutamiJ, HosoiA, NojiS, KurachiM, et al. (2010) Efficient cross-presentation of soluble exogenous antigens introduced into dendritic cells using a weak-based amphiphilic peptide. Biochem Biophys Res Commun 392 : 217–222.
21. TeszGJ, AouadiM, ProtM, NicoloroSM, BoutetE, et al. (2011) Glucan particles for selective delivery of siRNA to phagocytic cells in mice. Biochem J 436 : 351–362.
22. TamerisMD, HatherillM, LandryBS, ScribaTJ, SnowdenMA, et al. (2013) Safety and efficacy of MVA85A, a new tuberculosis vaccine in infants previously vaccinated with BCG: a randomized, placebo-controlled phase 2b trial. Lancet 381 : 1021–1028.
23. RappuoliR, MandlCW, BlackS, De GregorioE (2011) Vaccines for the twenty-first century society. Nat Rev Immunol 11 : 865–872.
24. MorganEL, ThomanML, SandersonSD, PhillipsJA (2010) A novel adjuvant for vaccine development in the aged. Vaccine 28 : 8275–8279.
25. LivingstonB, CrimiC, NewmanM, HigashimotoY, AppellaE, et al. (2002) A rational strategy to design multiepitope immunogens based on multiple Th lymphocyte epitopes. J Immunol 168 : 5499–5506.
26. YanoA, OnozukaA, Asahi-OzakiY, ImaiS, HanadaN, et al. (2005) An ingenious design for peptide vaccines. Vaccine 23 : 2322–2326.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Parental Transfer of the Antimicrobial Protein LBP/BPI Protects Eggs against Oomycete InfectionsČlánek Immune Therapeutic Strategies in Chronic Hepatitis B Virus Infection: Virus or Inflammation Control?Článek Coronaviruses as DNA Wannabes: A New Model for the Regulation of RNA Virus Replication FidelityČlánek CRISPR-Cas Immunity against Phages: Its Effects on the Evolution and Survival of Bacterial PathogensČlánek The Cyst Wall Protein CST1 Is Critical for Cyst Wall Integrity and Promotes Bradyzoite PersistenceČlánek The Malarial Serine Protease SUB1 Plays an Essential Role in Parasite Liver Stage Development
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2013 Číslo 12- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Host Susceptibility Factors to Bacterial Infections in Type 2 Diabetes
- LysM Effectors: Secreted Proteins Supporting Fungal Life
- Influence of Mast Cells on Dengue Protective Immunity and Immune Pathology
- Innate Lymphoid Cells: New Players in IL-17-Mediated Antifungal Immunity
- Cytoplasmic Viruses: Rage against the (Cellular RNA Decay) Machine
- Balancing Stability and Flexibility within the Genome of the Pathogen
- The Evolution of Transmissible Prions: The Role of Deformed Templating
- Parental Transfer of the Antimicrobial Protein LBP/BPI Protects Eggs against Oomycete Infections
- Host Defense via Symbiosis in
- Regulatory Circuits That Enable Proliferation of the Fungus in a Mammalian Host
- Immune Therapeutic Strategies in Chronic Hepatitis B Virus Infection: Virus or Inflammation Control?
- Burning Down the House: Cellular Actions during Pyroptosis
- Coronaviruses as DNA Wannabes: A New Model for the Regulation of RNA Virus Replication Fidelity
- CRISPR-Cas Immunity against Phages: Its Effects on the Evolution and Survival of Bacterial Pathogens
- Combining Regulatory T Cell Depletion and Inhibitory Receptor Blockade Improves Reactivation of Exhausted Virus-Specific CD8 T Cells and Efficiently Reduces Chronic Retroviral Loads
- Shaping Up for Battle: Morphological Control Mechanisms in Human Fungal Pathogens
- Identification of the Virulence Landscape Essential for Invasion of the Human Colon
- Nodular Inflammatory Foci Are Sites of T Cell Priming and Control of Murine Cytomegalovirus Infection in the Neonatal Lung
- Hepatitis B Virus Disrupts Mitochondrial Dynamics: Induces Fission and Mitophagy to Attenuate Apoptosis
- Mycobacterial MazG Safeguards Genetic Stability Housecleaning of 5-OH-dCTP
- Systematic MicroRNA Analysis Identifies ATP6V0C as an Essential Host Factor for Human Cytomegalovirus Replication
- Placental Syncytium Forms a Biophysical Barrier against Pathogen Invasion
- The CD8-Derived Chemokine XCL1/Lymphotactin Is a Conformation-Dependent, Broad-Spectrum Inhibitor of HIV-1
- Cyclin A Degradation by Primate Cytomegalovirus Protein pUL21a Counters Its Innate Restriction of Virus Replication
- Genome-Wide RNAi Screen Identifies Novel Host Proteins Required for Alphavirus Entry
- Zinc Sequestration: Arming Phagocyte Defense against Fungal Attack
- The Cyst Wall Protein CST1 Is Critical for Cyst Wall Integrity and Promotes Bradyzoite Persistence
- Biphasic Euchromatin-to-Heterochromatin Transition on the KSHV Genome Following Infection
- The Malarial Serine Protease SUB1 Plays an Essential Role in Parasite Liver Stage Development
- HIV-1 Vpr Accelerates Viral Replication during Acute Infection by Exploitation of Proliferating CD4 T Cells
- A Human Torque Teno Virus Encodes a MicroRNA That Inhibits Interferon Signaling
- The ArlRS Two-Component System Is a Novel Regulator of Agglutination and Pathogenesis
- An In-Depth Comparison of Latent HIV-1 Reactivation in Multiple Cell Model Systems and Resting CD4+ T Cells from Aviremic Patients
- Enterohemorrhagic Hemolysin Employs Outer Membrane Vesicles to Target Mitochondria and Cause Endothelial and Epithelial Apoptosis
- Overcoming Antigenic Diversity by Enhancing the Immunogenicity of Conserved Epitopes on the Malaria Vaccine Candidate Apical Membrane Antigen-1
- The Type-Specific Neutralizing Antibody Response Elicited by a Dengue Vaccine Candidate Is Focused on Two Amino Acids of the Envelope Protein
- Tmprss2 Is Essential for Influenza H1N1 Virus Pathogenesis in Mice
- Signatures of Pleiotropy, Economy and Convergent Evolution in a Domain-Resolved Map of Human–Virus Protein–Protein Interaction Networks
- Interference with the Host Haemostatic System by Schistosomes
- RocA Truncation Underpins Hyper-Encapsulation, Carriage Longevity and Transmissibility of Serotype M18 Group A Streptococci
- Gene Fitness Landscapes of at Important Stages of Its Life Cycle
- Phagocytosis Escape by a Protein That Connects Complement and Coagulation Proteins at the Bacterial Surface
- t Is a Structurally Novel Crohn's Disease-Associated Superantigen
- An Increasing Danger of Zoonotic Orthopoxvirus Infections
- Myeloid Dendritic Cells Induce HIV-1 Latency in Non-proliferating CD4 T Cells
- Transcriptional Analysis of Murine Macrophages Infected with Different Strains Identifies Novel Regulation of Host Signaling Pathways
- Serotonergic Chemosensory Neurons Modify the Immune Response by Regulating G-Protein Signaling in Epithelial Cells
- Genome-Wide Detection of Fitness Genes in Uropathogenic during Systemic Infection
- Induces an Unfolded Protein Response via TcpB That Supports Intracellular Replication in Macrophages
- Intestinal CD103+ Dendritic Cells Are Key Players in the Innate Immune Control of Infection in Neonatal Mice
- Emerging Functions for the RNome
- KSHV MicroRNAs Mediate Cellular Transformation and Tumorigenesis by Redundantly Targeting Cell Growth and Survival Pathways
- HrpA, an RNA Helicase Involved in RNA Processing, Is Required for Mouse Infectivity and Tick Transmission of the Lyme Disease Spirochete
- A Toxin-Antitoxin Module of Promotes Virulence in Mice
- Real-Time Imaging of the Intracellular Glutathione Redox Potential in the Malaria Parasite
- Hypoxia Inducible Factor Signaling Modulates Susceptibility to Mycobacterial Infection via a Nitric Oxide Dependent Mechanism
- Novel Strategies to Enhance Vaccine Immunity against Coccidioidomycosis
- Dual Expression Profile of Type VI Secretion System Immunity Genes Protects Pandemic
- —What Makes the Species a Ubiquitous Human Fungal Pathogen?
- αvβ6- and αvβ8-Integrins Serve As Interchangeable Receptors for HSV gH/gL to Promote Endocytosis and Activation of Membrane Fusion
- -Induced Activation of EGFR Prevents Autophagy Protein-Mediated Killing of the Parasite
- Semen CD4 T Cells and Macrophages Are Productively Infected at All Stages of SIV infection in Macaques
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Influence of Mast Cells on Dengue Protective Immunity and Immune Pathology
- Host Defense via Symbiosis in
- Coronaviruses as DNA Wannabes: A New Model for the Regulation of RNA Virus Replication Fidelity
- Myeloid Dendritic Cells Induce HIV-1 Latency in Non-proliferating CD4 T Cells
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



