-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaBroad-Spectrum Anti-biofilm Peptide That Targets a Cellular Stress Response
Bacteria colonize most environments, including the host by forming biofilms, which are extremely (adaptively) resistant to conventional antibiotics. Biofilms cause at least 65% of all human infections, being particularly prevalent in device-related infections, infections on body surfaces and in chronic infections. Currently there is a severe problem with antibiotic-resistant organisms, given the explosion of antibiotic resistance whereby our entire arsenal of antibiotics is gradually losing effectiveness, combined with the paucity of truly novel compounds under development or entering the clinic. Thus the even greater resistance of biofilms adds to the major concerns being expressed by physicians and medical authorities. Consequently, there is an urgent need for new strategies to treat biofilm infections and we demonstrate in the present study an approach, based on the inhibition of (p)ppGpp by a small peptide, that eradicates biofilms formed by four of the so-called ESKAPE pathogens, identified by the Infectious Diseases Society of America as the most recalcitrant and resistant organisms in our society. The strategy presented here represents a significant advance in the search for new agents that specifically target bacterial biofilms.
Published in the journal: . PLoS Pathog 10(5): e32767. doi:10.1371/journal.ppat.1004152
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1004152Summary
Bacteria colonize most environments, including the host by forming biofilms, which are extremely (adaptively) resistant to conventional antibiotics. Biofilms cause at least 65% of all human infections, being particularly prevalent in device-related infections, infections on body surfaces and in chronic infections. Currently there is a severe problem with antibiotic-resistant organisms, given the explosion of antibiotic resistance whereby our entire arsenal of antibiotics is gradually losing effectiveness, combined with the paucity of truly novel compounds under development or entering the clinic. Thus the even greater resistance of biofilms adds to the major concerns being expressed by physicians and medical authorities. Consequently, there is an urgent need for new strategies to treat biofilm infections and we demonstrate in the present study an approach, based on the inhibition of (p)ppGpp by a small peptide, that eradicates biofilms formed by four of the so-called ESKAPE pathogens, identified by the Infectious Diseases Society of America as the most recalcitrant and resistant organisms in our society. The strategy presented here represents a significant advance in the search for new agents that specifically target bacterial biofilms.
Introduction
Biofilms are structured multicellular communities of microorganisms associated with surfaces. They have been widely studied, in part because they cause at least 65% of all human infections, being particularly prevalent in device-related infections, on body surfaces (skin and soft tissue, lung, bladder, endocarditis, etc.) and in chronic infections [1], [2]. They represent a major health problem worldwide due to their resistance to host defence mechanisms and to conventional antimicrobials, which generally target free-swimming (planktonic) bacteria [1], [2]. Hence, there is an urgent need to identify compounds that effectively clear biofilm-related infections.
Bacteria are known to respond to stressful environmental conditions (such as starvation) by activating the stringent response (SR) [3]. As a consequence, the cell synthesizes two small signaling nucleotides, guanosine 5′-diphosphate 3′-diphosphate (ppGpp) and guanosine 5′-triphosphate 3′-diphosphate (pppGpp), collectively denoted (p)ppGpp [3]. These serve as a second messenger response that is induced by a variety of stress conditions, is highly conserved in both Gram-negative and Gram-positive species [3], [4], regulates the expression of a plethora of genes [3], and is known to play a role in biofilm formation in certain species [5]–[11], although some variability has been observed [6], [7], [9], [12].
Synthetic cationic peptides, derived from natural peptides such as the human cathelicidin LL-37 and the bovine peptide indolicidin [13], have been recently identified as biofilm inhibitory compounds [14]. Anti-biofilm peptides are similar to cationic antimicrobial peptides (which are active against planktonic bacteria), comprising both cationic and hydrophobic amino acids [14], but have substantially different structure-activity relationships. Thus, we previously identified peptides with good anti-biofilm but virtually no activity vs. planktonic bacteria (i.e., very high MIC values) [14], and vice versa. Moreover, certain anti-biofilm peptides are active against biofilms formed by Burkholderia cenocepacia [14], a pathogen that is completely resistant to all antimicrobial peptides in the planktonic state. The broad-spectrum activity of anti-biofilm peptides [14] suggests that they target a biofilm-specific process common amongst bacteria. Given the above, we hypothesized that anti-biofilm peptides exerted their activity by blocking a widespread stress response that contributes to biofilm development, and that this was indeed the stringent response mediated through (p)ppGpp. Here, we have identified a peptide that has very broad spectrum activity against many of the most antibiotic-resistant species of concern in human medicine and provide evidence it acts to promote (p)ppGpp degradation.
Results
Peptide 1018 as a potent broad-spectrum anti-biofilm agent
While screening for peptides with anti-biofilm activity, we identified the previously unknown ability of the immunomodulatory peptide IDR (innate defense regulator)-1018 (VRLIVAVRIWRR-NH2; abbreviated here as 1018) [15] to specifically target and kill biofilm cells (Fig. 1), at much lower concentrations than previously described peptides [14]. At concentrations that had no effect on planktonic growth (Table 1), this peptide was able to potently prevent biofilm formation (Fig. 1, middle panels) and eradicate preformed (2-day old) biofilms (Fig. 1, right hand panels) formed by diverse species of Gram-negative bacteria and the Gram-positive bacterium Staphylococcus aureus.
Fig. 1. Peptide 1018 potently inhibited bacterial biofilms at concentrations that did not affect planktonic cell growth. 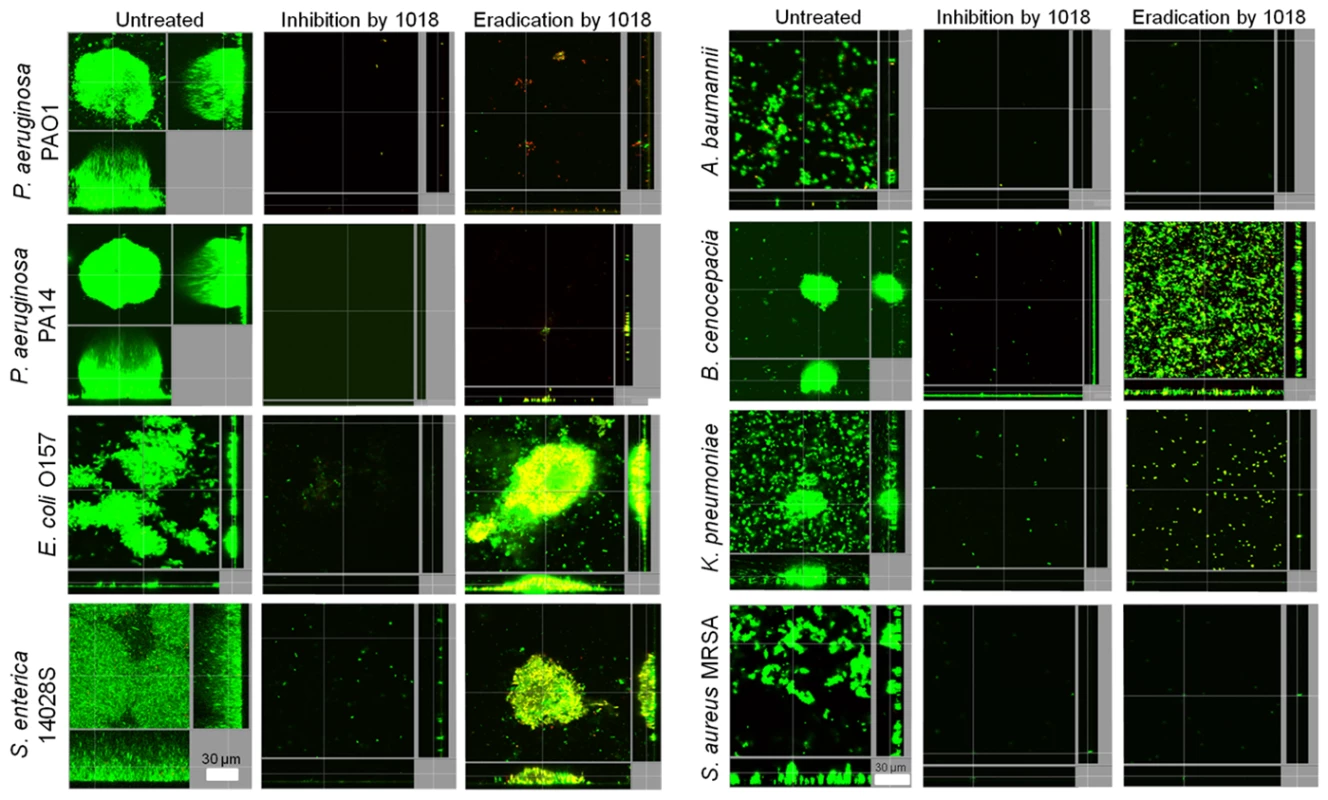
Sub-inhibitory concentrations of peptide 1018 prevented biofilm development and eradicated or reduced existing biofilms of Gram-negative and Gram-positive bacteria. Concentrations of peptide 1018 used were 10 µg/ml for Pseudomonas aeruginosa (labelled as strains PA14 and PAO1) Escherichia coli 0157, Acinetobacter baumannii and Burkholderia cenocepacia, 20 µg/ml for Salmonella enterica serovar Typhimurium 14028S experiments, 2 µg/ml for Klebsiella pneumoniae experiments, and 2.5 µg/ml for methicillin resistant Staphylococcus aureus (MRSA) experiments. Inhibition of biofilm development was tested by immediately adding 1018 into the flow-through medium of the flow cell apparatus and then monitoring biofilm formation for 3 days. Eradication conditions involved waiting two days before addition of 1018 into the flow-through medium. After 3 days, bacteria were stained green with the all bacteria stain Syto-9 and red with the dead-bacteria stain propidium iodide (merge shows as yellow to red) prior to confocal imaging. Each panel shows reconstructions from the top in the large panel and sides in the right and bottom panels (xy, yz and xz dimensions). Tab. 1. Peptide 1018 exhibited potent broad-spectrum direct anti-biofilm activity but weak antibacterial activity for planktonic cells. 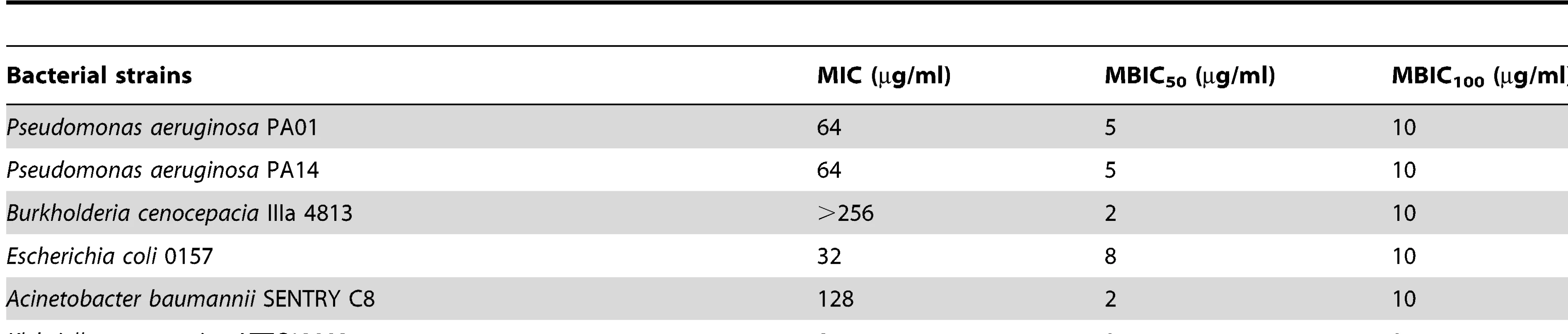
Comparison of planktonic cell MIC to MBIC50 and MBIC100, which are the minimal biofilm inhibitory concentrations leading to 50% and 100% decrease in biofilm growth, respectively. We investigated the role of 1018 in biofilm cell dispersion and killing of P. aeruginosa PA14 2-day old biofilms. At very low concentrations (0.8 µg/ml), the peptide increased live cell dispersion from existing biofilms by ∼4-fold after 23 h of treatment (Fig. 2), resulting in an average of 8.2±6.6% residual biofilm biovolume compared to the untreated controls (P<0.05). Only 26±7.4% of the cells that remained attached within the flow cell chambers were killed by treatment with 0.8 µg/ml 1018. Conversely, higher concentrations of peptide (10 µg/ml) did not trigger live biofilm cell dispersal (Fig. 2), and most of the cells remaining bound to the surface were dead, as judged by uptake of the normally impermeant stain propidium iodide (67±7.7% red cells compared to 2.5±1.0% in the untreated controls; P<0.05).
Fig. 2. Low levels of 1018 led to biofilm dispersion while higher levels triggered biofilm cell death. 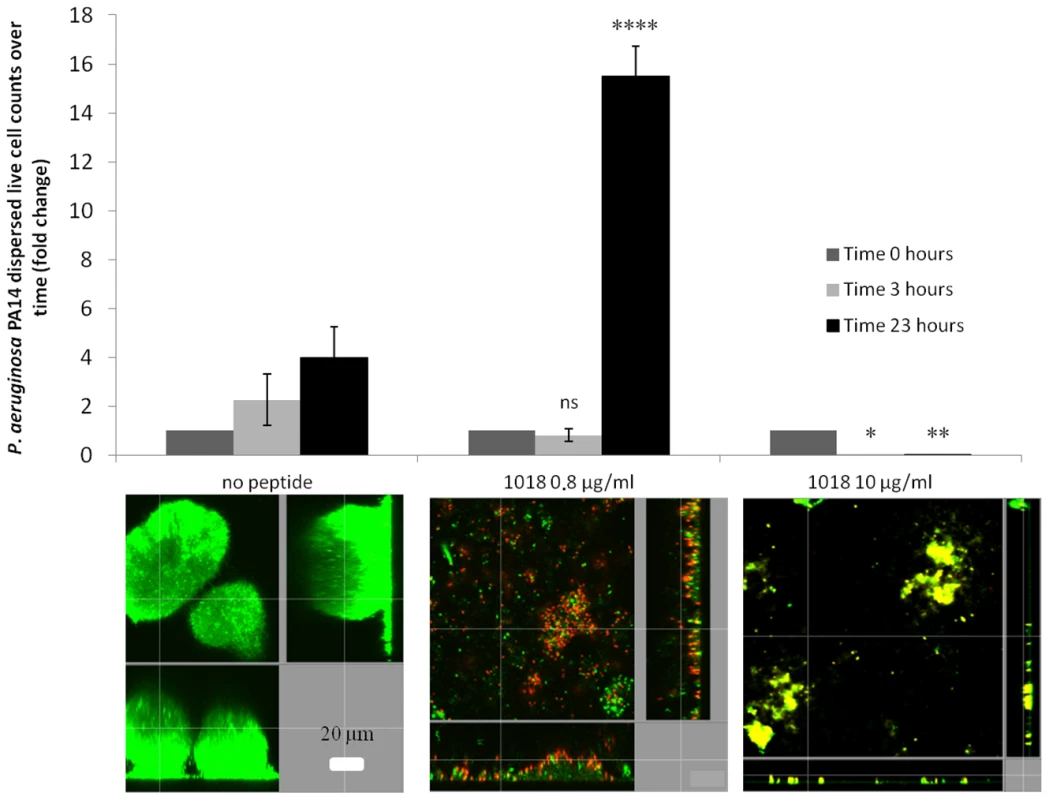
Dispersed cells from mature P. aeruginosa flow cell biofilms were collected and viable cell counts performed after 0, 3 and 23 h of treatment with different concentrations of the peptide (0.8 and 10 µg/ml). Representative confocal images of the remaining cells present in the flow cell chambers after peptide treatment are shown for each condition. Statistical significance comparing peptide-treated groups to untreated was determined using Student's t test (ns, P>0.05; *, P<0.05; **, P<0.01; ****, P<0.0001). In experiments with pre-grown, 2-day old biofilms, only E. coli 0157, S. enterica 14028S and B. cenocepacia samples consistently had attached cells after peptide treatment (Fig. 1, right hand panels). However, the remaining cell population was mostly dead in the case of E. coli 0157 as, on average, there was a significant increase in dead cell number in treated samples (54.4±3.1%) compared to untreated samples (1.5±0.9%; P<0.05). On the other hand, the peptide caused more substantial dispersal but lesser cell death in S. enterica 14028S and B. cenocepacia biofilms. Salmonella biofilms treated with 1018 had 29.2±19.0% dead cells as opposed to just 0.54±0.69% in samples without peptide (P<0.05). B. cenocepacia biofilms exhibited no significant increase in cell death (7.9±3.4% cf. 3.8±2.4% in the untreated controls).
Evidence for a role for the stringent response
The basis for the broad-spectrum activity of peptide 1018 was investigated. Previous studies, based on transcriptomic and biochemical investigations, have suggested that peptides LL-37 [13] and 1037 [14] act against Pseudomonas by modestly inhibiting attachment and quorum sensing as well as promoting twitching motility. However, although we could show that 1018 had similar modest effects on these processes, it was difficult to rationalize these mechanisms with the observed broad-spectrum activity, since these processes vary substantially within the above-described target species. Thus we considered that there might be a common mechanism and hypothesized that the peptide acted to inhibit a common stress response in target species, namely the so-called stringent response, mediating (p)ppGpp synthesis through the enzymes RelA and SpoT.
Overproducing the potential target of a given drug is a well-established method for identifying drug targets. Here we overproduced (p)ppGpp by addition of serine hydroxamate (SHX; a structural analogue of L-serine that induces the stringent response by inhibiting charging of seryl-tRNA synthetase [16]), and by IPTG induction of the cloned relA gene, and observed resistance against peptide 1018 (Fig. 3A,B). First we performed checkerboard microtiter plate assays, using established methods [17], to analyze the interaction between SHX addition at time 0 and 1018 treatment in more detail. Minor modifications were made to previously described methodology [17] to quantify adherent biofilm biomass (as opposed to planktonic bacterial growth) using the crystal violet assay [14]. The crystal violet-stained biofilm was resuspended using 70% ethanol and quantified using a spectrophotometer at 595 nm. Three independent experiments were performed and statistical significance was determined using Student's t test. At concentrations of SHX (10 µM) that did not affect P. aeruginosa PAO1 planktonic growth (which required 250 µM SHX to inhibit growth, Fig. S1C), we observed increased biofilm formation by nearly 2-fold (to 188±0.3% cf. the SHX untreated control; P<0.05). In these cells the minimal biofilm inhibitory concentration (MBIC) went from 10 µg/ml (Table 1) to 80 µg/ml of 1018 (leading to a reduction to 8.9±0.02% biofilm volume cf. the peptide untreated control; P<0.05; no difference was observed at 40 µg/ml of the peptide, which led to 93.2±0.04% biofilm formation cf. the peptide untreated control). These results clearly showed that peptide resistance was not due to slow growth. At 320 µM SHX, whereby biofilm production was increased nearly 4-fold (to 395±0.4% cf. the SHX untreated control; P<0.01), 160 µg/ml 1018 was required to fully inhibit biofilm formation (reduced to 4.7±0.002% cf. peptide untreated control; P<0.01). Thus the amount of peptide required to inhibit biofilms depended on the concentration of SHX, and therefore on the levels of (p)ppGpp, since increasing the levels of SHX resulted in peptide resistance unless a higher dose of peptide was used. While SHX by itself clearly resulted in an increase in biofilm development over the 18 to 24 h of the assay, the peptide was present in these studies even before biofilms began to develop.
Fig. 3. Enhanced (p)ppGpp production leads to altered susceptibility of biofilms to peptides. 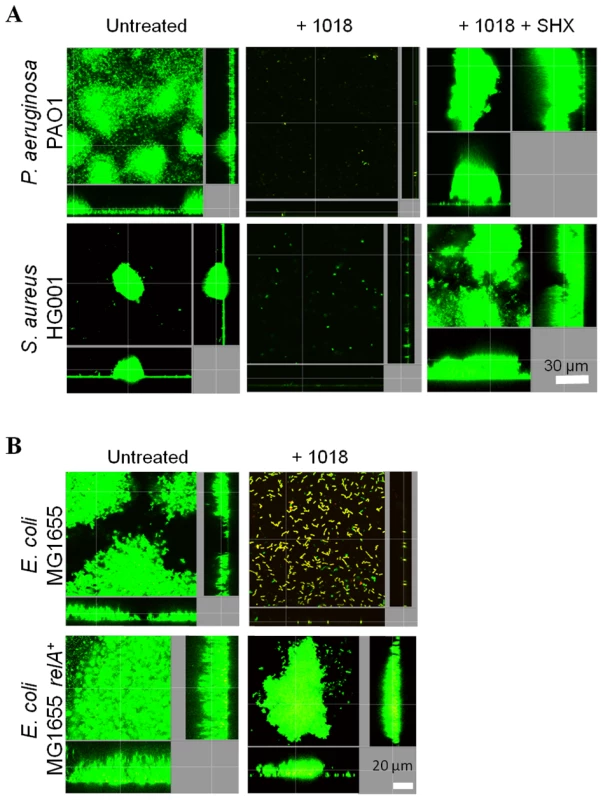
(A) Addition of SHX, which leads to overproduction of (p)ppGpp, resulted in the resistance of biofilm development to 20 µg/ml of peptide 1018; (B) (p)ppGpp overproduction through relA overexpression led to anti-biofilm peptide resistance. (A–B) Inhibition of biofilm development was tested by immediately adding 20 µg/ml 1018 (± SHX or IPTG) into the flow-through medium of the flow cell apparatus and then monitoring biofilm formation for 3 days. After 3 days, bacteria were stained green with the all bacteria stain Syto-9 prior to confocal imaging. Each panel shows reconstructions from the top in the large panel and sides in the right and bottom panels (xy, yz and xz dimensions). These results were confirmed and extended using flow cell methods. Overproduction of (p)ppGpp by SHX treatment of P. aeruginosa and S. aureus wild-type strains led to peptide resistance (Fig. 3A). The fold-change in biovolume of P. aeruginosa PAO1 biofilms treated with 20 µg/ml 1018 was 0.095±0.03 (P<0.05) compared to untreated controls. However, adding SHX restored the ability to form biofilms in the presence of the peptide (2.6±0.5 fold-increase compared to untreated samples; P<0.05). Similarly, the biovolume of 1018-treated S. aureus HG001 biofilms was only 0.6% that of untreated samples, which was complemented when adding SHX (1.65±0.6 fold-change compared to untreated samples; P<0.05). Similar results were obtained by genetic means whereby peptide resistance was increased by overproduction of (p)ppGpp in an E. coli strain overexpressing the cloned relA gene under the control of an IPTG-inducible promoter (Fig. 3B).
Evidence for (p)ppGpp as an important signal in biofilm growth
Previous studies have reported that mutants influencing (p)ppGpp production are biofilm-deficient but not always completely defective, occasionally forming monolayers of attached cells or extremely-deficient biofilms (as opposed to well-structured biofilms) [7]–[11]. To confirm that there was a correlation between the production of (p)ppGpp and biofilm production under the experimental conditions reported here, biofilm formation of (p)ppGpp-deficient mutants was compared to their respective wild-type strains in Gram-negative Pseudomonas aeruginosa, Salmonella enterica serovar Typhimurium, and Escherichia coli and the Gram-positive bacterium Staphylococcus aureus (Fig. 4, Fig. S1A). Cells unable to synthesize (p)ppGpp showed a substantial decrease in their ability to adhere tightly to the plastic surface of flow cell chambers and were unable to develop structured biofilms, although they formed residual aggregates (Fig. 4, Fig. S1A). Genetic complementation of the genes responsible for (p)ppGpp synthesis in P. aeruginosa relA spoT and S. aureus rsh mutants restored the full ability to form biofilms (Fig. 4). In the un-complemented mutants (Fig. 4, Fig. S1A), residual (p)ppGpp-deficient mutant cells appeared to be in the planktonic state as opposed to adhering to the surface, and often were dead or division-inhibited (demonstrating filaments) (Fig. S1B). These poorly-attached cells could be cleared by increasing the flow rate. This might explain in part the variability in the defect in biofilm formation in mutants defective in (p)ppGpp production (i.e. due to flow rate, or other factors such as the age of the biofilms, temperature and media utilized here, which differed compared to previous reports; 6,7,9,12).
Fig. 4. Genetic complementation of (p)ppGpp synthetase enzymes restored the ability to form biofilms. 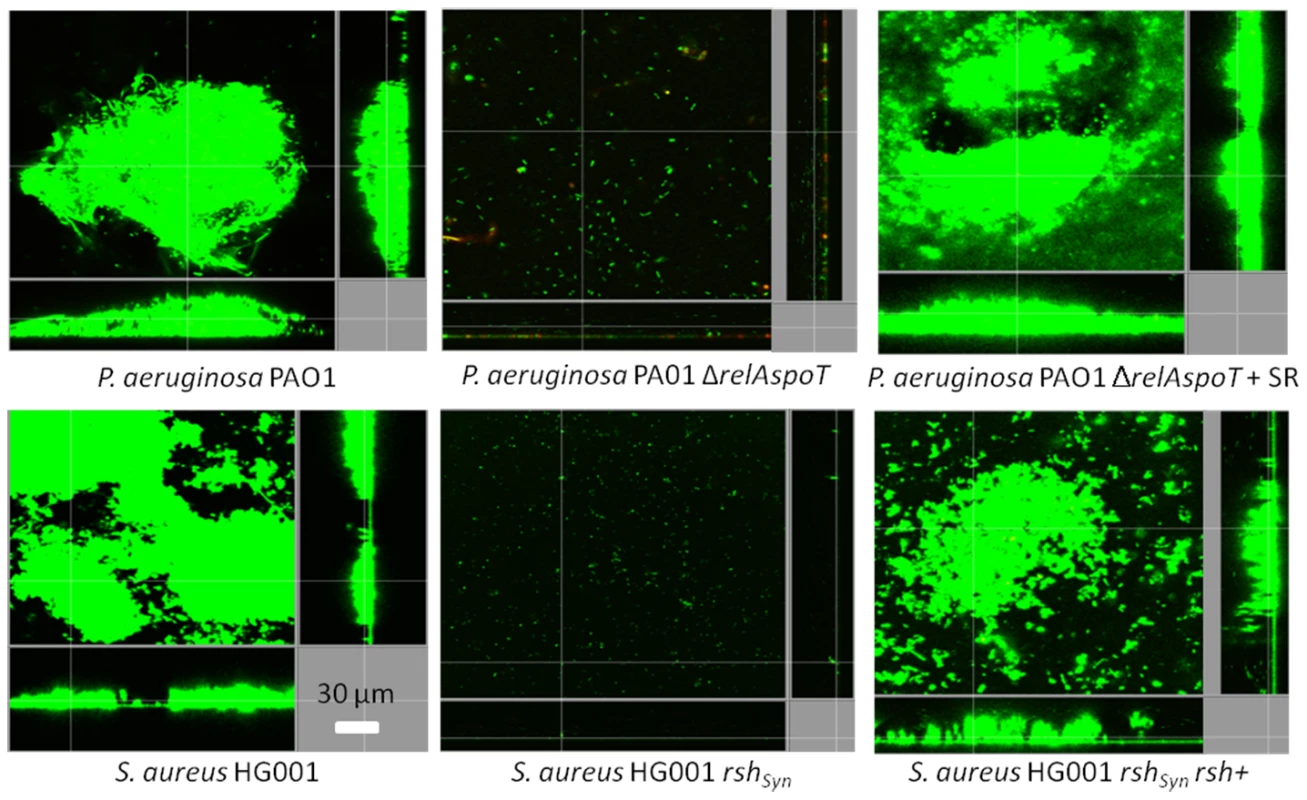
The biofilm deficiency of Pseudomonas aeruginosa PAO1 and Staphylococcus aureus HG001 (p)ppGpp mutants (ΔrelAspoT and rshSyn respectively) was rescued by genetic complementation [ΔrelAspoT + relAspoT+ (+SR) as described [12] and rsh+ [30], respectively] leading to biofilm formation equivalent to WT shown in the left-most panels. After 3 days, bacteria were stained green with the all bacteria stain Syto-9 and red with the dead-bacteria stain propidium iodide (merge shows as yellow to red) prior to confocal imaging. Each panel shows reconstructions from the top in the large panel and sides in the right and bottom panels (xy, yz and xz dimensions). To further demonstrate the role of (p)ppGpp in biofilm development and maintenance, we introduced the relA gene under the control of an araC promoter into P. aeruginosa PAO1ΔrelAspoT such that it expressed relA upon arabinose induction. Biofilms of this strain that were expressing relA due to the introduction of arabinose into the flow medium during the 3-day experiment, were able to form well-structured biofilms (Fig. 5A). However, when induction of relA was stopped at day 2 (i.e. for the last 24 h of the experiment by removal of arabinose from the flow medium), analogous to delayed treatment by peptide 1018, pre-formed biofilms were dispersed (Fig. 5A). Indeed, we performed viable cell counts of dispersed cells from these biofilms and found that repressing relA expression after 2 days of continuous induction led to biofilm dispersion (Fig. 5B), while continued induction of relA for the 3 days of the experiment resulted in significantly reduced dispersal levels (Fig. 5B) that were similar to that of the wild-type strain (data not shown). These results clearly highlighted the roles that relA-dependent (p)ppGpp production play both in biofilm formation and in biofilm maintenance, as well as the consequences of blocking (p)ppGpp synthesis.
Fig. 5. Modulation of relA expression impacts on biofilm development. 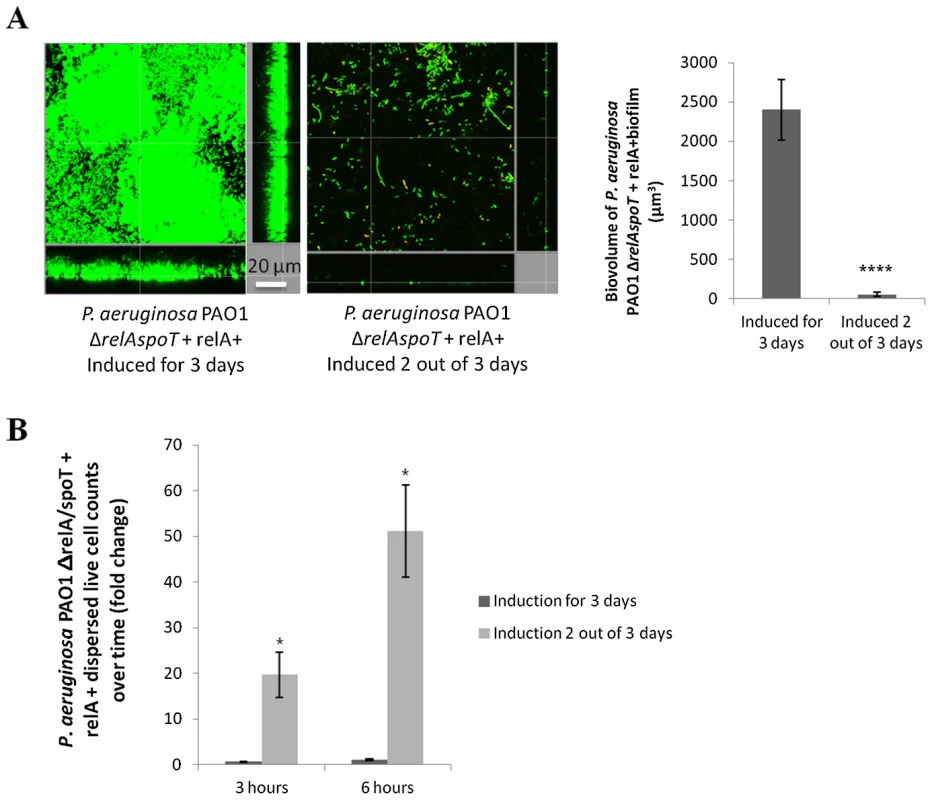
(A) relA expression modulated biofilm formation and disassembly. The relA gene under the control of an arabinose-inducible promoter was introduced into a P. aeruginosa PAO1 ΔrelAspoT background. Induction of relA led to biofilm formation in flow cells after 3 days. On the other hand, induction of relA for 2 days followed by 24 h of non-induction led to biofilm dispersal. Biofilm biovolume was calculated using Imaris software from Bitplane AG. Experiments were performed at least in triplicate. Student's t test was used (****, P<0.0001). (B) Repression of relA expression (after 2 days of induction) led to biofilm dispersal in a P. aeruginosa PAO1 ΔrelAspoT strain, while continuous induction of relA expression during the 3 days of the experiment resulted in significantly fewer cells dispersed from biofilms. Dispersed cells from 2-day old biofilms were collected and viable cell counts performed 3 and 6 h after induction of relA expression was either stopped or continued. Statistical significance was determined using Student's t test (*, P<0.05). Involvement of (p)ppGpp in 1018 action
The role of (p)ppGpp in the anti-biofilm mechanism of peptide 1018 was further assessed in multiple species. Direct measurement of the cellular levels of (p)ppGpp by thin layer chromatography (TLC) revealed that cells from multiple bacterial species treated with 5 µg/ml of peptide 1018 did not accumulate (p)ppGpp (Fig. 6A and Fig. S4B). In contrast, the conventional cationic antibiotics colistin, polymyxin B and tobramycin were unable to prevent (p)ppGpp accumulation (Fig. S3, left panel; indeed the latter two actually increased ppGpp) or cause degradation of accumulated (p)ppGpp (Fig. S3, right panel), thus demonstrating that these cationic antibiotics did not utilize a similar mechanism to that of peptide 1018.
Fig. 6. Peptide 1018 prevented (p)ppGpp accumulation in vivo as revealed by thin layer chromatography separation of guanine nucleotides extracted from intact cells. 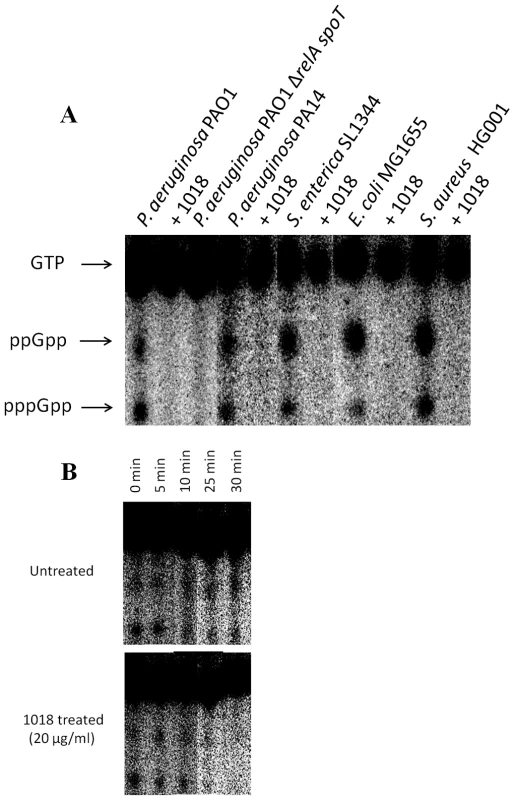
(A) Anti-biofilm peptide 1018 at 5 µg/ml directly prevented (p)ppGpp accumulation. (B) Treatment with peptide 1018 led to (p)ppGpp elimination within 30 min in P. aeruginosa PAO1 cells containing pre-accumulated (p)ppGpp due to SHX treatment. In panel A, bacteria were grown overnight in modified MOPS minimal medium containing 0.4% glucose, 2 mM phosphate (KH2PO4), and 0.2% CAA. For experiments evaluating the ability of the peptide to directly degrade (p)ppGpp in panel B, the cells were grown as described previously, induced with SHX and allowed to synthesize (p)ppGpp for 3 h prior to peptide treatment. After growth for both A and B, the cells were then diluted 1∶20 in the same MOPS minimal medium except containing 0.4 mM phosphate (KH2PO4) and 500 µM serine hydroxamate (SHX) to induce (p)ppGpp synthesis, in the presence or absence of peptide 1018 and cells were labelled with 10 µCi/ml 32P for 3 h. Samples were then extracted with frozen 13 M formic acid by three cycles of freeze-thaw. Aliquots of the supernatants were applied to 20×20 cm PEI cellulose TLC plates, resolved with 1.5 M KH2PO4, pH 3.4 for 4 h. After chromatography, nucleotides were visualized by autoradiography and quantified with a MolecularImager FX PhosphorImager and Quantity One software (Bio-Rad). Controls were performed to demonstrate that the ΔrelAspoT mutation also prevented (p)ppGpp formation. The peptide was able to interact directly with ppGpp as demonstrated by co-precipitation (Fig. 7A) and TLC of residual ppGpp (Fig. 6, Fig. S4B) and by nuclear magnetic resonance spectrometry (NMR) of the complexed molecules (Fig. 7B–D). These studies further showed that peptide 1018 preferentially bound to ppGpp compared to other nucleotides such as GTP (Fig. 7A, Fig. S5B).
Fig. 7. Peptide 1018 bound to ppGpp in vitro and led to degradation of (p)ppGpp in vivo. 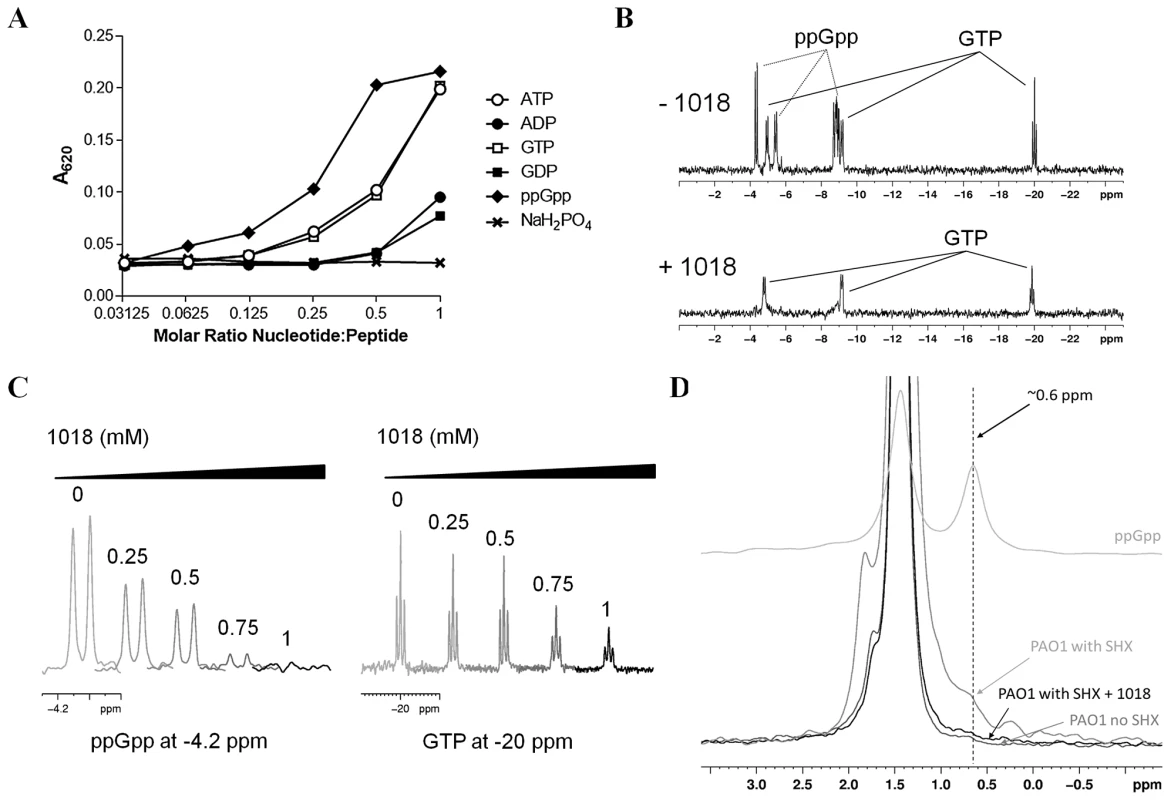
(A) Binding of peptide 1018 to various nucleotides based on co-precipitation. Peptide 1018 (0.25 mM) was separately mixed with increasing amounts of ppGpp, GTP, ATP, GDP and ADP in buffer (50 mM Tris, pH 7.4) and the extent of co-precipitation was assessed by measuring the increase in absorbance at 620 nm. The amount of co-precipitation induced by 1018 appeared to correlate with an increased negative charge on the nucleotides. A separate sample containing NaH2PO4 revealed that phosphate ions did not induce precipitation of 1018 in the concentration range tested. (B) Anti-biofilm peptide 1018 preferentially bound to ppGpp compared to GTP as revealed by 31P-NMR spectroscopy. In the absence of 1018 (top panel), a mixture of 0.5 mM ppGpp and 0.5 mM GTP revealed unique signals corresponding to the phosphorous atoms in ppGpp and GTP (indicated by arrows). Upon the addition of 1 mM 1018 (bottom panel), the peak intensity from the ppGpp signals was almost completely abolished, while the signals from GTP were reduced but to a lesser degree. (C) Samples containing an equimolar mixture of ppGpp and GTP at intermediate concentrations of 1018 were used to further evaluate the preferential binding of 1018 to ppGpp. Examination of specific spectral regions unique to 31P signals from either ppGpp (∼−4.2 ppm) or GTP (∼−20 ppm) showed that the ppGpp peak intensity decreased more readily than those from GTP (peptide concentrations, in mM, are indicated above each trace). The preferential precipitation of ppGpp by 1018 suggests that the peptide had a higher affinity for ppGpp over GTP under these conditions (See also Fig. S5B). (D) The ppGpp levels in nucleotide extracts from P. aeruginosa PAO1 cultures induced with SHX and treated with 1018 were also measured using 31P-NMR spectroscopy. In these spectra, the ppGpp phosphorous signals were shifted because of the presence of 6.5 M formic acid used to extract the nucleotides from the PAO1 cells. The chemical shifts of GTP and ppGpp in 6.5 M formic acid were determined separately using samples of pure nucleotide (See Fig. S6). Only the region from 3 ppm to −0.5 ppm is shown as this contained a unique ppGpp phosphorous peak at 0.6 ppm (for comparison, the spectra of 0.5 mM ppGpp in 6.5 M formic acid is shown as the top trace). In the 31P spectrum of nucleotide extracts from PAO1 induced with SHX, the ppGpp peak at 0.6 ppm appeared as a shoulder on the large phosphate peak at 1.5 ppm (middle grey trace). This shoulder was absent in samples taken from PAO1 cells grown without SHX (lowest grey trace). When PAO1 induced with SHX was treated with 20 µg/ml 1018, the ppGpp peak was essentially lost (black trace) demonstrating that the addition of 1018 to bacteria leads to the degradation of ppGpp in vivo. We then investigated the mechanism by which the peptide 1018-ppGpp interaction led to the loss of the ppGpp signal in cells. One possibility was that the peptide sequestered the nucleotide, forming a peptide-ppGpp complex, which prevented ppGpp detection in our TLC and NMR assays. However, we observed that formic acid (used to extract nucleotides in both TLC and NMR experiments) led to a disruption of the peptide-ppGpp complex while maintaining ppGpp in its intact form (Fig. S5A, right panel), so this explanation seems unlikely as no ppGpp was visible on TLC and NMR after formic acid treatment (Fig. 6, Fig. 7D, Fig. S5A). Alternatively, peptide treatment could lead to ppGpp degradation. In agreement with this second possibility, TLC and NMR analysis of in vivo experiments showed that the addition of peptide led to the rapid degradation of (p)ppGpp within cells that had pre-accumulated these nucleotides (Fig. 6B, Fig. 7D). In the TLC experiments, (p)ppGpp synthesis was induced in P. aeruginosa PAO1 cultures by SHX for 3 h, after which 20 µg/ml of the peptide was added and the fate of (p)ppGpp was monitored over time, revealing elimination within only 30 min (Fig. 6B). Likewise, after treatment with SHX to induce (p)ppGpp synthesis in P. aeruginosa PAO1 cells and then treatment with peptide for 1 h followed by extraction of nucleotides and NMR, the ppGpp peak observed in untreated cells was dramatically reduced (Fig. 7D). Taken together, these results indicate that peptide 1018 directly and specifically interacts with (p)ppGpp and triggers its degradation, thus preventing its signaling effects within the cell (e.g. its role in biofilm development and maintenance).
Discussion
The results described here indicate that an anti-biofilm peptide can exhibit potent broad-spectrum activity due to its ability to depress (p)ppGpp levels in live bacterial cells. Previous studies have suggested that the stringent response might be involved in biofilm formation [5]–[11], although some controversy exists as to whether this may be due to the particular experimental conditions used, particularly flow rate and age of the biofilms examined. The stringent response is induced in reaction to bacterial stresses such as amino-acid starvation, fatty acid, iron or nutritional limitation, heat shock, and other stress conditions. It is signaled by the alarmone (p)ppGpp, and modulates transcription of up to one third of all genes in the cell. Conceptually it is designed to divert resources away from growth and division and toward metabolism in order to promote survival. Its specific role in biofilm formation is not known but it may be involved in initiating and/or perpetuating biofilm development. In addition, the results presented here indicate that it may actually suppress the tendency of biofilms to disperse (Fig. 5), and even promote viability in adhered cells (Fig. S1B). Consistent with its effects on biofilms, in vivo studies have shown that (p)ppGpp-deficient mutants are easily cleared by the host, unable to establish chronic infections, incapable of long-term survival and overall more susceptible to exogenous stresses than their parent strains [18], [19]. Interestingly, various classes of antibiotics are known to induce (p)ppGpp synthesis [20-23; Fig. S3], which in turn leads to antibiotic adaptive resistance [12], [24]. Importantly, recent efforts have identified molecules that target the stringent response [25].
Here we have demonstrated that peptide 1018, which triggers the degradation of the (p)ppGpp signal within the cell, acts as a broad-spectrum biofilm inhibitor. Given the importance of biofilms in human medicine, constituting at least 65% of all infections, and increasing antibiotic resistance which in biofilms is adaptive and broad spectrum, such a peptide offers considerable potential in the fight against the burgeoning resistance to antibiotics. Peptides with biofilm inhibitory activities have been previously identified [13], [14], [26]. However, the mechanism of action by which these peptides selectively target and kill biofilm cells of both Gram-negative and Gram-positive bacteria was previously postulated to involve changes in motility, adherence and quorum sensing [13], [14], which are all species-specific and thus do not satisfactorily explain the action of peptide 1018 against a broad range of pathogens. Here we provide evidence that an anti-biofilm peptide, 1018, potently inhibited biofilm formation and eradicated existing mature biofilms in a broad-spectrum manner, through a direct interaction with ppGpp, which led to its degradation in live bacterial cells. The mechanism of action involves direct contact between peptide 1018 and (p)ppGpp so the peptide must be able to cross the cell membranes to reach the cytoplasm. Previous studies have demonstrated that amphipathic cationic peptides, like 1018, have the characteristics of so-called cell penetrating peptides that are able to freely translocate across membranes [27].
The peptide had at least three effects on biofilms, which might reflect the role of (p)ppGpp in cells. First when added prior to initiation of biofilms it prevented biofilm formation, second it specifically led to cell death in biofilms at concentrations that were not lethal for planktonic (free-swimming) cells (Table 1; Figs. 1 and 2), and third it promoted biofilm dispersal even in maturing (2-day old) biofilms (Fig. 2), effects that were in fact reciprocated in mutants unable to accumulate (p)ppGpp (Fig. 5). We suggest that the ability to cause cell death in biofilms might have been due to inhibition of cell wall biosynthesis and triggering of murine hydrolases, a known tendency for antimicrobial peptides [28]. Critically we propose that this is due in part to the impact of the stringent response in bacteria growing in the biofilm state, since stringent response is known to influence susceptibility to cell wall specific antibiotics, presumably through effects on cell wall synthesis [24], while the lack of ppGpp leads to cell death through the Slt soluble lytic transglycosylase [29]. Consistent with this, both peptide-treated biofilms and (p)ppGpp deficient mutants grown in flow cells demonstrated increased bacterial cell filamentation (Fig. S1B) and cell lysis/death (Figs. 1, 2, S1B and Fig. 5).
Previous studies have demonstrated that the structure-activity relationships of anti-biofilm peptides vary substantially from antimicrobial peptides [14] despite certain common features (being amphipathic molecules with excess cationic and hydrophobic amino acids). Consistent with this, 1018 was able to potently inhibit Burkholderia cenocepacia biofilms, despite the fact that this species is completely resistant to all antimicrobial peptides. Thus we have an opportunity to now develop more active peptides that have even more potent anti-biofilm activity. Indeed we have recently started to isolate such peptides and obtained preliminary evidence that they also act by inhibiting the stringent response.
Materials and Methods
Bacterial strains
Strains utilized included wild-type strains of Pseudomonas aeruginosa PAO1, strain H103, and PA14 and clinical isolates E. coli O157, Salmonella enterica serovar Typhimurium (clinical isolate 14028S), Staphylococcus aureus MRSA (clinical isolate #SAP0017), Klebsiella pneumoniae ATTC 13883 (a colistin-heteroresistant reference strain from American Type Culture Collection, Rockville, MD), Acinetobacter baumannii SENTRY C8 (a polymyxin B resistant blood clinical isolate from the U.S.A. obtained through the SENTRY surveillance system) and Burkholderia cenocepacia genomovar IIIa (Vancouver Children's Hospital clinical isolate 4813). P. aeruginosa PAO1 (p)ppGpp mutant ΔrelAspoT [(ΔrelA (Δ181-2019) ΔspoT (Δ200-1948)] and its complemented strain ΔrelAspoT+SR were a kind gift from D. Nguyen [12]. S. aureus parent strain HG001, its (p)ppGpp mutant HG001 rshsyn (Δ942–950 nt) and the strain complemented with full length rsh were kindly provided by T. Geiger [30]. S. enterica serovar Typhimurium parent strain SL1344 and its (p)ppGpp mutant SL1344 ΔrelAspoT (ΔrelA71::kan rpsL ΔspoT281::cat) were provided by K. Tedin [31]. Escherichia coli parent strain (MG1655), E. coli ΔrelAspoT [ΔrelA:: kan (Δ209-2302) ΔspoT:: cat (Δ700-2355)] deletion insertion mutant and E. coli relA+ (p)ppGpp positive control ptac::relA (pALS10) were also provided by D. Nguyen and obtained as previously described [32], [33]. For the expression of relA in the P. aeruginosa mutant strain PAO1ΔrelAspoT, the pHERD20T plasmid carrying an arabinose-inducible promoter was used [34]. A 3.2 kb DNA fragment containing the relA gene was amplified with primers relAF (5'-GCTAGGATGCCTGCGTAATC-3') and relAR (5'-GAGATCGCCATCGAGGAATA-3') and cloned into a TOPO Zero-Blunt cloning vector (Invitrogen) and then into the pHERD20T vector. This construct was then electroporated into electrocompetent P. aeruginosa PAO1ΔrelAspoT cells. Positives clones carrying the plasmid were selected on LB plus 500 µg/ml of carbenicillin, and relA overexpression upon induction was confirmed by RT-qPCR. In all experiments 0.01% arabinose was used to induce the promoter.
Peptide synthesis
Peptide 1018 (VRLIVAVRIWRR-NH2) used in this study was synthesized by CPC Scientific using solid-phase 9-fluorenylmethoxy carbonyl (Fmoc) chemistry and purified to a purity of ∼95% using reverse-phase high-performance liquid chromatography (HPLC). Peptide mass was confirmed by mass spectrometry.
Growth conditions
The medium used was generally BM2 minimal medium (62 mM potassium phosphate buffer, pH 7.0, 7 mM [(NH4)2SO4, 2 mM MgSO4, 10 µM FeSO4] containing 0.4% (wt/vol) glucose as a carbon source, except for Staphylococcus aureus HG001 wild-type for which BM2 glucose+0.5% casamino acids (CAA) was used, and Salmonella enterica SL1344 that was grown in Luria Broth. Escherichia coli MG1655 was grown in BM2+0.1% CAA.
Minimal Inhibitory Concentration (MIC, MBIC50, MBIC100) assays
The broth microdilution method with minor modifications for cationic peptides [35] was used for measuring the MIC of peptide 1018. Minimal biofilm inhibitory concentrations leading to 50% decrease in biofilm growth (MBIC50) were obtained using 96-well plate assays and crystal violet staining of adherent biofilms as previously described [14]. The minimal peptide concentrations that completely inhibited biofilm formation (MBIC100) were obtained using flow cells at different input concentrations of peptide.
Biofilm cultivation in flow cell chambers and microscopy
Biofilms were grown in flow chambers with channel dimensions of 1×4×40 mm, as previously described for 72 h at 37°C [14] in the absence or presence of the desired concentration of peptide 1018. Flow cell chambers were inoculated by injecting 400 µl of an overnight culture diluted to an OD600 of 0.05. After inoculation, chambers were left without flow for 2 h to enable initial adherence, after which the medium (with or without sub-inhibitory concentrations of 1018) was pumped through the system at a constant rate of 2.4 ml/h. In all cases, after 3 days of growth the flow rate (90 rpm) was increased so as to limit the amount of planktonic and loosely-attached cells within the flow cell chamber. All media used (see above) in flow cell assays supported the planktonic growth of the bacterial species tested, as determined by growth curves (e.g. Fig. S1A). Except where otherwise specified, the concentrations of peptide 1018 used were 10 µg/ml for Pseudomonas aeruginosa, Escherichia coli 0157, Acinetobacter baumannii SENTRY C8 and Burkholderia cenocepacia genomovar IIIa 4813, 20 µg/ml for Salmonella enterica sv. Typhimurium 14028S experiments, 2 µg/ml for Klebsiella pneumoniae ATTC13883, and 2.5 µg/ml for methicillin resistant Staphylococcus aureus MRSA #SAP0017. The different concentrations used correspond to the MBIC100 of the peptide against the different bacterial species as shown in Table 1. For inhibition studies, peptide was added to the flow-through medium immediately after the initial adherence phase, and maintained for 3 days. For treatment of existing biofilms, bacteria were allowed to develop into structured 2-day old biofilms prior to peptide treatment by addition into the flow cell flow-through medium for the following 24 h. Biofilm cells were stained using the LIVE/DEAD BacLight Bacterial Viability kit (Molecular Probes, Eugene, OR) or Syto-9 alone prior to microscopy experiments. A ratio of Syto-9 (green fluorescence, live cells) to propidium iodide (PI) (red fluorescence, dead cells) of 1∶5 was used. Microscopy was done using a confocal laser scanning microscope (Olympus, Fluoview FV1000) and three-dimensional reconstructions were generated using the Imaris software package (Bitplane AG). Quantification of the overall biofilm biovolume (µm3) and the percentage of live and dead cell volume were performed using Imaris software as previously described [7], [36]. Experiments were performed at least in triplicate.
In experiments looking at the effect of enhanced (p)ppGpp production of biofilm susceptibility to peptides, E. coli strain MG1655 expressing relA from a lac promoter on plasmid pALSl0 [32] was grown in flow cells for 3 days in BM2+0.1% CAA containing 20 µg/ml of 1018 and in the presence or absence of 100 µM isopropyl β-D-1-thiogalactopyranoside (IPTG). P. aeruginosa PAO1 and S. aureus HG001 strains were grown as described above but in the presence or absence of serine hydroxamate (SHX).
Dispersal biofilm cell assay
Cell counts of live dispersed bacteria from flow cell biofilms were performed using strain P. aeruginosa PA14 grown in BM2 minimal glucose medium. P. aeruginosa PA14 biofilms were grown in the flow cell system for 2 days as described above and treated with 0.8 µg/ml or 10 µg/ml of peptide 1018. To count the dispersed viable cells, 1.5 ml of the output flow was collected at the designated times (time 0 and after 3 and 23 h) and serially diluted 10-fold. One hundred-µl portions from these serial dilutions were then plated onto LB agar plates. Plates were incubated at 37°C overnight, and colony counts were performed to obtain total CFU/ml at each time point.
(p)ppGpp measurement by thin layer chromatography
Bacteria were grown overnight in modified MOPS minimal medium containing 0.4% glucose, 2 mM phosphate (KH2PO4), and 0.2% CAA. The cells were then diluted 1∶20 in the same MOPS minimal medium except containing 0.4 mM phosphate (KH2PO4) and 500 µM SHX to induce (p)ppGpp synthesis, in the presence or absence of peptide 1018, colistin, tobramycin or polymyxin B and cells were labelled with 10 µCi/ml 32P for 3 h. For experiments evaluating the ability of the peptide (or different antibiotics) to directly lead to degradation of (p)ppGpp, the cells were induced with SHX and allowed to synthesize (p)ppGpp (for 3 h) prior to peptide treatment. Samples were then extracted with frozen 13 M formic acid by three cycles of freeze-thaw. Aliquots (7.5 µl) of the supernatants were applied to 20×20 cm PEI cellulose TLC plates, resolved with 1.5 M KH2PO4 (pH 3.4) for 4 h. After chromatography, nucleotides were visualized by autoradiography and quantified with a MolecularImager FX PhosphorImager and Quantity One software (Bio-Rad). Unlabeled GTP was spotted on the plates as markers and visualized after chromatography by UV light-induced fluorescence.
Nucleotide co-precipitation
The ability of 1018 to co-precipitate with nucleotides with varying phosphate content was examined as described previously by Hilpert et al. [37]. Peptide 1018 was mixed separately with ppGpp, GTP, GDP, ATP, ADP or NaH2PO4 in 50 mM Tris buffer at pH 7.4. ppGpp was purchased from TriLink BioTechnologies and all other nucleotides were purchased from Sigma. Nucleotide concentrations ranging from 0.25 to 0.008 mM were mixed in a microtiter plate with 0.25 nmoles of 1018 in a final volume of 100 µl per well. Samples were also prepared containing only 1018 or the nucleotide of interest at each concentration. The co-precipitation of 1018 with a nucleotide resulted in an increase in turbidity, which was quantified by measuring the A620 using a Powerwave X 340 microplate reader (BioTek Instruments Inc., Winooski, VT, USA).
31P-NMR spectroscopy
31P-NMR spectroscopy was used to evaluate the binding of 1018 to ppGpp and GTP. Samples containing 0.5 mM GTP or ppGpp were prepared in buffer (10 mM Tris, 50 mM NaCl, pH 7.4) and 1 mM phosphate was added as an internal chemical shift reference as well as for quantification. Separate samples containing 0.5 mM 1018 mixed with each nucleotide were prepared in the same way. Additional samples of 0.5 mM ppGpp, GTP and ATP with 1 mM phosphate were also prepared in 6.5 M formic acid for comparison to the samples prepared from the P. aeruginosa PAO1 extracts (see below). All samples contained 10% D2O. Each NMR sample was briefly centrifuged on a benchtop centrifuge (∼30 s) to pellet any precipitate that formed and the supernatant liquid was used as the NMR sample. 31P spectra were acquired at 25 °C on a Bruker Avance 500 MHz spectrometer, operating at a 31P frequency of 202.272 MHz. A single pulse experiment, with a 90 degree pulse of 20 µs was used, on a BB 500 probe. 4096 scans were acquired for the pure nucleotide samples while 12288 scans were accumulated for samples that contained peptide. Spectra were processed with an exponential window and line broadening of 50 Hz. To evaluate the differential binding of 1018 to ppGpp or GTP, samples containing an equimolar mixture of ppGpp and GTP (both at 0.5 mM) were prepared in Tris buffer. Peptide 1018 was added to separate nucleotide mixtures to achieve final peptide concentrations of 0.25, 0.5, 0.75 and 1 mM. The samples were again centrifuged to pellet the precipitate and the resulting supernatant was used in the NMR experiments. The experiments were performed as above, but the spectra were processed with a shifted sine bell window only. The phosphorous peak signal intensity resulting from unique chemical shift peaks from either ppGpp or GTP was determined at every concentration of 1018 tested.
To examine the effect of 1018 on ppGpp levels in vivo, 3×20 ml cultures of PAO1 (in BM2 media with 0.5% casamino acids) were grown overnight at 37°C in the presence of SHX (500 µM) to induce the production of ppGpp. Following overnight incubation, 1018 was added to a final concentration of 20 µg/ml and the sample was grown for an additional hour at 37°C. For comparison, a separate culture was prepared with no 1018 added. The PAO1 cells were harvested by centrifugation for 20 min at ∼2000×g in a Beckman Coulter Allegra 6 centrifuge. All three bacterial pellets were resuspended in a total of 400 µl H2O. To prepare the NMR sample, 400 µl of the bacteria suspension was added to 500 µl of 13 M formic acid and 100 µl of D2O. The sample was subjected to three rounds of freezing and thawing using liquid nitrogen and a room temperature water bath. The sample was centrifuged at 4°C and 14000 rpm in a microcentrifuge and 500 µl of the resulting supernatant was used as the NMR sample. Spectra were acquired as described for the pure nucleotide samples but with an accumulation of 24576 scans.
Supporting Information
Zdroje
1. CostertonJW, StewartPS, GreenbergEP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284 : 1318–22.
2. de la Fuente-NúñezC, ReffuveilleF, FernándezL, HancockREW (2013) Bacterial biofilm development as a multicellular adaptation: antibiotic resistance and new therapeutic strategies. Curr Opin Microbiol 16 : 580–9.
3. PotrykusK, CashelM (2008) (p)ppGpp: still magical? Annu Rev Microbiol 62 : 35–51.
4. MagnussonLU, FarewellA, NyströmT (2005) ppGpp: a global regulator in Escherichia coli. Trends Microbiol 13 : 236–42.
5. AbergA, ShinglerV, BalsalobreC (2006) (p)ppGpp regulates type 1 fimbriation of Escherichia coli by modulating the expression of the site-specific recombinase FimB. Mol Microbiol 60 : 1520–33.
6. BalzerGJ, McLeanRJ (2002) The stringent response genes relA and spoT are important for Escherichia coli biofilms under slow-growth conditions. Can J Microbiol 48 : 675–80.
7. Chávez de PazLE, LemosJA, WickströmC, SedgleyCM (2012) Role of (p)ppGpp in biofilm formation by Enterococcus faecalis. Appl Environ Microbiol 78 : 1627–30.
8. HeH, CooperJN, MishraA, RaskinDM (2012) Stringent response regulation of biofilm formation in Vibrio cholerae. J Bacteriol 194 : 2962–72.
9. LemosJA, BrownTAJr, BurneRA (2004) Effects of RelA on key virulence properties of planktonic and biofilm populations of Streptococcus mutans. Infect Immun 72 : 1431–40.
10. SugisakiK, HanawaT, YonezawaH, OsakiT, FukutomiT, et al. (2013) Role of (p)ppGpp in biofilm formation and expression of filamentous structures in Bordetella pertussis. Microbiology 159 : 1379–89.
11. TaylorCM, BeresfordM, EptonHA, SigeeDC, ShamaG, et al. (2002) Listeria monocytogenes relA and hpt mutants are impaired in surface-attached growth and virulence. J Bacteriol 184 : 621–8.
12. NguyenD, Joshi-DatarA, LepineF, BauerleE, OlakanmiO, et al. (2011) Active starvation responses mediate antibiotic tolerance in biofilms and nutrient-limited bacteria. Science 334 : 982–6.
13. OverhageJ, CampisanoA, BainsM, TorfsEC, RehmBH, et al. (2008) Human host defense peptide LL-37 prevents bacterial biofilm formation. Infect Immun 76 : 4176–82.
14. de la Fuente-NúñezC, KorolikV, BainsM, NguyenU, BreidensteinEB, et al. (2012) Inhibition of bacterial biofilm formation and swarming motility by a small synthetic cationic peptide. Antimicrob Agents Chemother 56 : 2696–704.
15. Rivas-SantiagoB, Castañeda-DelgadoJE, Rivas SantiagoCE, WaldbrookM, González-CurielI, et al. (2013) Ability of innate defence regulator peptides IDR-1002, IDR-HH2 and IDR-1018 to protect against Mycobacterium tuberculosis infections in animal models. PLoS One 8: e59119.
16. TosaT, PizerLI (1971) Biochemical bases for the antimetabolite action of L-serine hydroxamate. J Bacteriol 106 : 972–82.
17. YanH, HancockREW (2001) Synergistic interactions between mammalian antimicrobial defense peptides. Antimicrob Agents Chemother 45 : 1558–60.
18. DahlJL, KrausCN, BoshoffHI, DoanB, FoleyK, et al. (2003) The role of RelMtb-mediated adaptation to stationary phase in long-term persistence of Mycobacterium tuberculosis in mice. Proc Natl Acad Sci U S A 100 : 10026–31.
19. VogtSL, GreenC, StevensKM, DayB, EricksonDL, et al. (2011) The stringent response is essential for Pseudomonas aeruginosa virulence in the rat lung agar bead and Drosophila melanogaster feeding models of infection. Infect Immun 79 : 4094–104.
20. ErlichH, LafflerT, GallantJ (1971) ppGpp formation in Escherichia coli treated with rifampicin. J Biol Chem 246 : 6121–3.
21. KhanSR, YamazakiH (1972) Trimethoprim-induced accumulation of guanosine tetraphosphate (ppGpp) in Escherichia coli. Biochem Biophys Res Commun 48 : 169–74.
22. CortayJC, CozzoneAJ (1983) Accumulation of guanosine tetraphosphate induced by polymixin and gramicidin in Escherichia coli. Biochim Biophys Acta 755 : 467–73.
23. IkeharaK, KamitaniE, KoarataC, OguraA (1985) Induction of stringent response by streptomycin in Bacillus subtilis cells. J Biochem 97 : 697–700.
24. GilbertP, CollierPJ, BrownMR (1990) Influence of growth rate on susceptibility to antimicrobial agents: biofilms, cell cycle, dormancy, and stringent response. Antimicrob Agents Chemother 34 : 1865–8.
25. WexselblattE, Oppenheimer-ShaananY, KaspyI, LondonN, Schueler-FurmanO, et al. (2012) Relacin, a novel antibacterial agent targeting the Stringent Response. PLoS Pathog 8: e1002925.
26. PompilioA, ScocchiM, PomponioS, GuidaF, Di PrimioA, et al. (2011) Antibacterial and anti-biofilm effects of cathelicidin peptides against pathogens isolated from cystic fibrosis patients. Peptides 32 : 1807–14.
27. FjellCD, HissJA, HancockREW, SchneiderG (2011) Designing antimicrobial peptides: form follows function. Nat Rev Drug Discov 11 : 37–51.
28. FriedrichCL, MoylesD, BeveridgeTJ, HancockREW (2000) Antibacterial action of structurally diverse cationic peptides on Gram-positive bacteria. Antimicrob Agents Chemother 44 : 2086–92.
29. BetznerAS, FerreiraLC, HöltjeJV, KeckW (1990) Control of the activity of the soluble lytic transglycosylase by the stringent response in Escherichia coli. FEMS Microbiol Lett 55 : 161–4.
30. GeigerT, GoerkeC, FritzM, SchäferT, OhlsenK, et al. (2010) Role of the (p)ppGpp synthase RSH, a RelA/SpoT homolog, in stringent response and virulence of Staphylococcus aureus. Infect Immun 78 : 1873–83.
31. TedinK, NorelF (2001) Comparison of DeltarelA strains of Escherichia coli and Salmonella enterica serovar Typhimurium suggests a role for ppGpp in attenuation regulation of branched-chain amino acid biosynthesis. J Bacteriol 183 : 6184–96.
32. SvitilAL, CashelM, ZyskindJW (1993) Guanosine tetraphosphate inhibits protein synthesis in vivo. A possible protective mechanism for starvation stress in Escherichia coli. J Biol Chem 268 : 2307–11.
33. XiaoH, KalmanM, IkeharaK, ZemelS, GlaserG, et al. (1991) Residual guanosine 3',5'-bispyrophosphate synthetic activity of relA null mutants can be eliminated by spoT null mutations. J Biol Chem 266 : 5980–90.
34. QiuD, DamronFH, MimaT, SchweizerHP, YuHD (2008) PBAD-based shuttle vectors for functional analysis of toxic and highly regulated genes in Pseudomonas and Burkholderia spp. and other bacteria. Appl Environ Microbiol 74 : 7422–6.
35. WiegandI, HilpertK, HancockREW (2008) Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc 3 : 163–75.
36. SunS, KjellebergS, McDougaldD (2013) Relative contributions of Vibrio polysaccharide and quorum sensing to the resistance of Vibrio cholerae to predation by heterotrophic protists. PLoS One 8: e56338.
37. HilpertK, McLeodB, YuJ, ElliottMR, RautenbachM, et al. (2010) Short cationic antimicrobial peptides interact with ATP. Antimicrob Agents Chemother 54 : 4480–3.
Štítky
Hygiena a epidemiologie Infekční lékařství Laboratoř
Článek Combined Systems Approaches Reveal Highly Plastic Responses to Antimicrobial Peptide Challenge inČlánek Two Novel Human Cytomegalovirus NK Cell Evasion Functions Target MICA for Lysosomal Degradation
Článek vyšel v časopisePLOS Pathogens
Nejčtenější tento týden
2014 Číslo 5- Jak souvisí postcovidový syndrom s poškozením mozku?
- Měli bychom postcovidový syndrom léčit antidepresivy?
- Farmakovigilanční studie perorálních antivirotik indikovaných v léčbě COVID-19
- 10 bodů k očkování proti COVID-19: stanovisko České společnosti alergologie a klinické imunologie ČLS JEP
-
Všechny články tohoto čísla
- Surveillance for Emerging Biodiversity Diseases of Wildlife
- The Emerging Role of Urease as a General Microbial Virulence Factor
- PARV4: An Emerging Tetraparvovirus
- Epigenetic Changes Modulate Schistosome Egg Formation and Are a Novel Target for Reducing Transmission of Schistosomiasis
- The Human Adenovirus E4-ORF1 Protein Subverts Discs Large 1 to Mediate Membrane Recruitment and Dysregulation of Phosphatidylinositol 3-Kinase
- A Multifactorial Role for Malaria in Endemic Burkitt's Lymphoma Pathogenesis
- Structural Basis for the Ubiquitin-Linkage Specificity and deISGylating Activity of SARS-CoV Papain-Like Protease
- Cathepsin-L Can Resist Lysis by Human Serum in
- Epstein-Barr Virus Down-Regulates Tumor Suppressor Expression
- BCA2/Rabring7 Targets HIV-1 Gag for Lysosomal Degradation in a Tetherin-Independent Manner
- The Evolutionarily Conserved Mediator Subunit MDT-15/MED15 Links Protective Innate Immune Responses and Xenobiotic Detoxification
- Suppressor of Cytokine Signaling 4 (SOCS4) Protects against Severe Cytokine Storm and Enhances Viral Clearance during Influenza Infection
- T Cell Inactivation by Poxviral B22 Family Proteins Increases Viral Virulence
- Dynamics of HIV Latency and Reactivation in a Primary CD4+ T Cell Model
- HIV and HCV Activate the Inflammasome in Monocytes and Macrophages via Endosomal Toll-Like Receptors without Induction of Type 1 Interferon
- Virus and Autoantigen-Specific CD4+ T Cells Are Key Effectors in a SCID Mouse Model of EBV-Associated Post-Transplant Lymphoproliferative Disorders
- Severe Acute Respiratory Syndrome Coronavirus Envelope Protein Ion Channel Activity Promotes Virus Fitness and Pathogenesis
- Squalene Synthase As a Target for Chagas Disease Therapeutics
- The Contribution of Viral Genotype to Plasma Viral Set-Point in HIV Infection
- Combined Systems Approaches Reveal Highly Plastic Responses to Antimicrobial Peptide Challenge in
- Anthrax Lethal Factor as an Immune Target in Humans and Transgenic Mice and the Impact of HLA Polymorphism on CD4 T Cell Immunity
- Ly49C-Dependent Control of MCMV Infection by NK Cells Is -Regulated by MHC Class I Molecules
- Two Novel Human Cytomegalovirus NK Cell Evasion Functions Target MICA for Lysosomal Degradation
- A Large Family of Antivirulence Regulators Modulates the Effects of Transcriptional Activators in Gram-negative Pathogenic Bacteria
- Broad-Spectrum Anti-biofilm Peptide That Targets a Cellular Stress Response
- Malaria Parasite Infection Compromises Control of Concurrent Systemic Non-typhoidal Infection via IL-10-Mediated Alteration of Myeloid Cell Function
- A Role for in Higher Order Structure and Complement Binding of the Capsule
- Hip1 Modulates Macrophage Responses through Proteolysis of GroEL2
- CD8 T Cells from a Novel T Cell Receptor Transgenic Mouse Induce Liver-Stage Immunity That Can Be Boosted by Blood-Stage Infection in Rodent Malaria
- Phosphorylation of KasB Regulates Virulence and Acid-Fastness in
- HIV-Infected Individuals with Low CD4/CD8 Ratio despite Effective Antiretroviral Therapy Exhibit Altered T Cell Subsets, Heightened CD8+ T Cell Activation, and Increased Risk of Non-AIDS Morbidity and Mortality
- A Novel Mechanism Inducing Genome Instability in Kaposi's Sarcoma-Associated Herpesvirus Infected Cells
- Structural and Biochemical Characterization Reveals LysGH15 as an Unprecedented “EF-Hand-Like” Calcium-Binding Phage Lysin
- Hepatitis C Virus Cell-Cell Transmission and Resistance to Direct-Acting Antiviral Agents
- Different Modes of Retrovirus Restriction by Human APOBEC3A and APOBEC3G
- TNFα and IFNγ but Not Perforin Are Critical for CD8 T Cell-Mediated Protection against Pulmonary Infection
- Large Scale RNAi Reveals the Requirement of Nuclear Envelope Breakdown for Nuclear Import of Human Papillomaviruses
- The Cytoplasmic Domain of Varicella-Zoster Virus Glycoprotein H Regulates Syncytia Formation and Skin Pathogenesis
- A New Class of Multimerization Selective Inhibitors of HIV-1 Integrase
- Are We There Yet? The Smallpox Research Agenda Using Variola Virus
- High-Efficiency Targeted Editing of Large Viral Genomes by RNA-Guided Nucleases
- Dynamic Functional Modulation of CD4 T Cell Recall Responses Is Dependent on the Inflammatory Environment of the Secondary Stimulus
- Bacterial Superantigens Promote Acute Nasopharyngeal Infection by in a Human MHC Class II-Dependent Manner
- Follicular Helper T Cells Promote Liver Pathology in Mice during Infection
- A Nasal Epithelial Receptor for WTA Governs Adhesion to Epithelial Cells and Modulates Nasal Colonization
- Unexpected Role for IL-17 in Protective Immunity against Hypervirulent HN878 Infection
- Human Cytomegalovirus Fcγ Binding Proteins gp34 and gp68 Antagonize Fcγ Receptors I, II and III
- Expansion of Murine Gammaherpesvirus Latently Infected B Cells Requires T Follicular Help
- Venus Kinase Receptors Control Reproduction in the Platyhelminth Parasite
- Molecular Signatures of Hemagglutinin Stem-Directed Heterosubtypic Human Neutralizing Antibodies against Influenza A Viruses
- The Downregulation of GFI1 by the EZH2-NDY1/KDM2B-JARID2 Axis and by Human Cytomegalovirus (HCMV) Associated Factors Allows the Activation of the HCMV Major IE Promoter and the Transition to Productive Infection
- Inactivation of Fructose-1,6-Bisphosphate Aldolase Prevents Optimal Co-catabolism of Glycolytic and Gluconeogenic Carbon Substrates in
- New Insights into Rotavirus Entry Machinery: Stabilization of Rotavirus Spike Conformation Is Independent of Trypsin Cleavage
- Prophenoloxidase Activation Is Required for Survival to Microbial Infections in
- SslE Elicits Functional Antibodies That Impair Mucinase Activity and Colonization by Both Intestinal and Extraintestinal Strains
- Timed Action of IL-27 Protects from Immunopathology while Preserving Defense in Influenza
- HIV-1 Envelope gp41 Broadly Neutralizing Antibodies: Hurdles for Vaccine Development
- The PhoP-Dependent ncRNA Mcr7 Modulates the TAT Secretion System in
- Cellular Superspreaders: An Epidemiological Perspective on HIV Infection inside the Body
- The Inflammasome Pyrin Contributes to Pertussis Toxin-Induced IL-1β Synthesis, Neutrophil Intravascular Crawling and Autoimmune Encephalomyelitis
- Papillomavirus Genomes Associate with BRD4 to Replicate at Fragile Sites in the Host Genome
- Integrative Functional Genomics of Hepatitis C Virus Infection Identifies Host Dependencies in Complete Viral Replication Cycle
- Co-assembly of Viral Envelope Glycoproteins Regulates Their Polarized Sorting in Neurons
- Targeting Membrane-Bound Viral RNA Synthesis Reveals Potent Inhibition of Diverse Coronaviruses Including the Middle East Respiratory Syndrome Virus
- Dual-Site Phosphorylation of the Control of Virulence Regulator Impacts Group A Streptococcal Global Gene Expression and Pathogenesis
- PLOS Pathogens
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Venus Kinase Receptors Control Reproduction in the Platyhelminth Parasite
- Dual-Site Phosphorylation of the Control of Virulence Regulator Impacts Group A Streptococcal Global Gene Expression and Pathogenesis
- Severe Acute Respiratory Syndrome Coronavirus Envelope Protein Ion Channel Activity Promotes Virus Fitness and Pathogenesis
- High-Efficiency Targeted Editing of Large Viral Genomes by RNA-Guided Nucleases
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



