-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPervasive Sharing of Genetic Effects in Autoimmune Disease
Genome-wide association (GWA) studies have identified numerous, replicable, genetic associations between common single nucleotide polymorphisms (SNPs) and risk of common autoimmune and inflammatory (immune-mediated) diseases, some of which are shared between two diseases. Along with epidemiological and clinical evidence, this suggests that some genetic risk factors may be shared across diseases—as is the case with alleles in the Major Histocompatibility Locus. In this work we evaluate the extent of this sharing for 107 immune disease-risk SNPs in seven diseases: celiac disease, Crohn's disease, multiple sclerosis, psoriasis, rheumatoid arthritis, systemic lupus erythematosus, and type 1 diabetes. We have developed a novel statistic for Cross Phenotype Meta-Analysis (CPMA) which detects association of a SNP to multiple, but not necessarily all, phenotypes. With it, we find evidence that 47/107 (44%) immune-mediated disease risk SNPs are associated to multiple—but not all—immune-mediated diseases (SNP-wise PCPMA<0.01). We also show that distinct groups of interacting proteins are encoded near SNPs which predispose to the same subsets of diseases; we propose these as the mechanistic basis of shared disease risk. We are thus able to leverage genetic data across diseases to construct biological hypotheses about the underlying mechanism of pathogenesis.
Published in the journal: . PLoS Genet 7(8): e32767. doi:10.1371/journal.pgen.1002254
Category: Research Article
doi: https://doi.org/10.1371/journal.pgen.1002254Summary
Genome-wide association (GWA) studies have identified numerous, replicable, genetic associations between common single nucleotide polymorphisms (SNPs) and risk of common autoimmune and inflammatory (immune-mediated) diseases, some of which are shared between two diseases. Along with epidemiological and clinical evidence, this suggests that some genetic risk factors may be shared across diseases—as is the case with alleles in the Major Histocompatibility Locus. In this work we evaluate the extent of this sharing for 107 immune disease-risk SNPs in seven diseases: celiac disease, Crohn's disease, multiple sclerosis, psoriasis, rheumatoid arthritis, systemic lupus erythematosus, and type 1 diabetes. We have developed a novel statistic for Cross Phenotype Meta-Analysis (CPMA) which detects association of a SNP to multiple, but not necessarily all, phenotypes. With it, we find evidence that 47/107 (44%) immune-mediated disease risk SNPs are associated to multiple—but not all—immune-mediated diseases (SNP-wise PCPMA<0.01). We also show that distinct groups of interacting proteins are encoded near SNPs which predispose to the same subsets of diseases; we propose these as the mechanistic basis of shared disease risk. We are thus able to leverage genetic data across diseases to construct biological hypotheses about the underlying mechanism of pathogenesis.
Introduction
The human immune-mediated diseases are the result of aberrant immune responses. These immune responses may lead to chronic inflammation and tissue destruction, often targeting a specific organ site. The outcome of this process is immune-mediated inflammatory and autoimmune disease, affecting approximately 5% of the population [1].
Extensive clinical and epidemiologic observations have shown that immune-mediated inflammatory and autoimmune diseases can occur either in the same individual or in closely related family members. This clustering of multiple diseases appears more frequently than expected if disease processes were independent. As each of the immune-mediated inflammatory and autoimmune diseases has strong genetic influences on disease risk [2]–[7], the observed clustering of multiple diseases could be due to an overlap in the causal genes and pathways [8], [9].
The patterns of clustering of diseases across the population are complex [10] – each disease has a prevalence between 0.01%–3%, so direct assessment of co-aggregation within individuals or families does not result in the very large samples required for genetic or epidemiological investigation. Thus it is unsurprising that to date, these observations have yet to be translated into determinants of the shared molecular etiologies of disease.
Recent GWA studies in immune-mediated and autoimmune diseases have identified 140 regions of the genome with statistically significant and robust evidence of presence of disease susceptibility loci. A subset of these loci have been shown to modulate risk of multiple diseases [3], [6], [11]–[14]. In addition, there is evidence that loci predisposing to one disease can have effects on risk of a second disease [15], although the risk allele for one disease may not be the same as for the second [16].
Together, these observations support the hypothesis of a common genetic basis of immune-mediated and autoimmune diseases [17]. There is now the ability to estimate both the number of loci contributing to risk of multiple diseases and the spectrum of diseases that each locus influences. In addition, grouping variants by the diseases they influence should provide insight into the specific biological processes underlying co-morbidity and disease risk.
In this report, we systematically investigate the genetic commonality in immune-mediated inflammatory and autoimmune diseases by examining the contributions of associated genomic risk regions in seven diseases: celiac disease (CeD), Crohn's disease (CD), multiple sclerosis (MS), psoriasis (Ps), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE) and type 1 diabetes (T1D). We find that nearly half of loci identified in GWAS studies of an individual disease influence risk to at least two diseases, arguing for a genetic basis to co-morbidity. We also find several variants with opposing risk profiles in different diseases. Supporting the idea that common patterns of association implicate shared biological processes, we further demonstrate that loci clustered by the pattern of diseases they affect harbor genes encoding interacting proteins at a much higher rate than by chance. These results suggest that multi-phenotype mapping will identify the molecular mechanisms underlying co-morbid immune-mediated inflammatory and autoimmune diseases.
Results
We first test our hypothesis of common genetic determinants by examining evidence of association of genetic variants in known immune-mediated and autoimmune disease susceptibility loci to multiple disease phenotypes. We collated a list of 140 single nucleotide polymorphisms (SNPs) representing reported associations to at least one immune-mediated disease at genome-wide significance levels. Where data for the reported SNP itself were not available in our GWA studies (Table 1), we chose a proxy in high linkage disequilibrium to the reported marker (r2>0.9 in HapMap/CEU). We did not consider SNPs in the human Major Histocompatibility Complex (MHC) from this analysis, as its role in many of these diseases is well-established and the classically associated alleles in the HLA region are not well captured by SNPs [18]. We were able to acquire data for either the reported SNP or a good proxy in 107 of 140 cases, and assembled genotype test summaries for these from previously described GWA studies representing over 26,000 disease cases (Table 1).
Tab. 1. Participating studies. 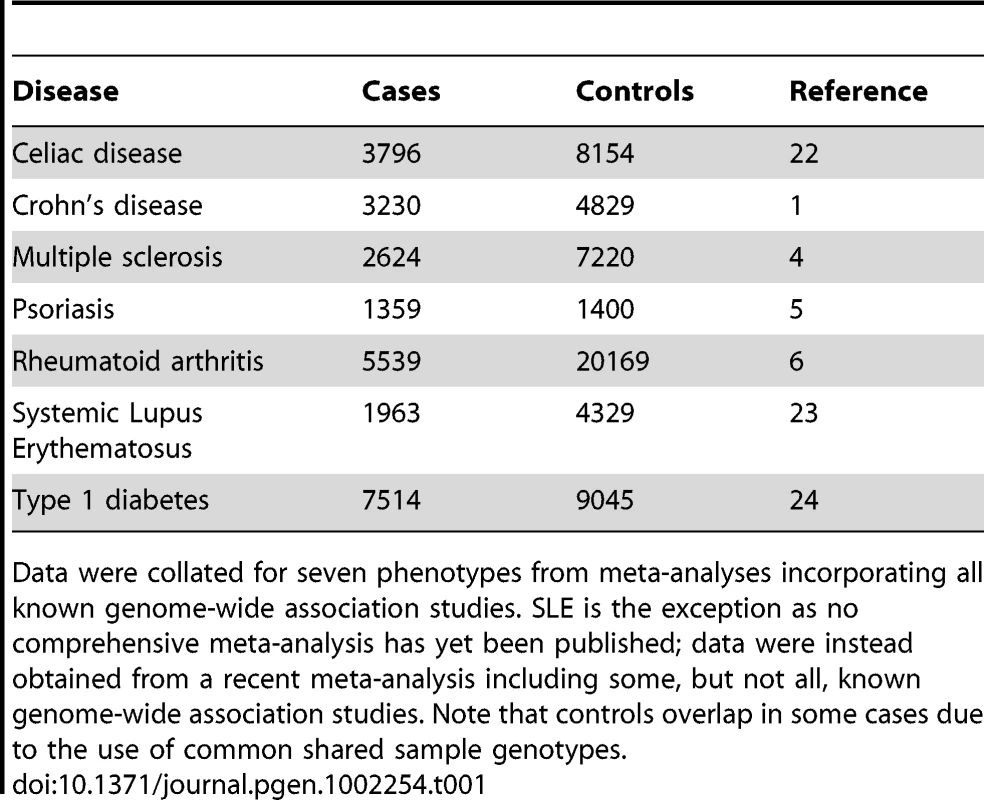
Data were collated for seven phenotypes from meta-analyses incorporating all known genome-wide association studies. SLE is the exception as no comprehensive meta-analysis has yet been published; data were instead obtained from a recent meta-analysis including some, but not all, known genome-wide association studies. Note that controls overlap in some cases due to the use of common shared sample genotypes. We have developed a cross-phenotype meta-analysis (CPMA) statistic to assess association across multiple phenotypes. The CPMA statistic determines evidence for the hypothesis that each independent SNP has multiple phenotypic associations. Support for this hypothesis would be shown by deviations from expected uniformity of the distribution of association p-values, indicative of multiple associations. The likelihood of the observed rate of exponential decay of −log10(p) is calculated and compared to the null expectation (the decay rate should be unity) as a likelihood ratio test (see Materials and Methods for details). This CPMA statistic has one degree of freedom, as it measures a deviation in p-value behavior instead of testing all possible combinations of diseases for association to each SNP.
A total of 47 of the 107 SNPs tested have evidence of association to multiple diseases (SNP-wise PCPMA<0.01; expectation roughly 1 by chance; binomial probability of observing this result p = 3×10−64). This highly significant result confirms widespread sharing of genetic loci between immune-mediated inflammatory and autoimmune diseases. Further, these “multi-phenotype” SNPs include many loci not previously known to be shared across diseases, as well as new predictions of association for previously known shared loci (Table 2).
Tab. 2. SNPs associated with multiple phenotypes. 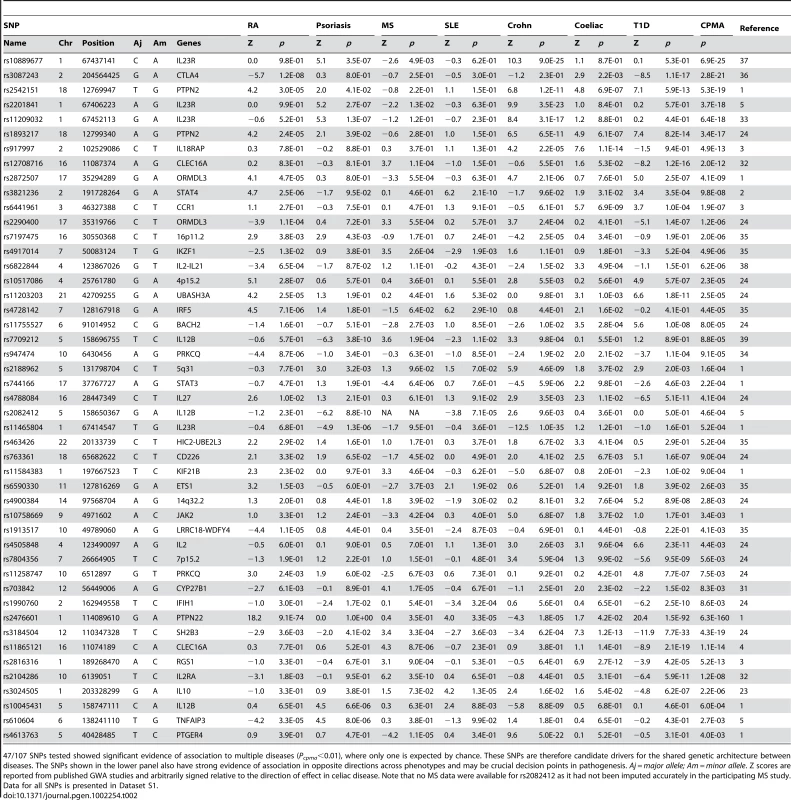
47/107 SNPs tested showed significant evidence of association to multiple diseases (Pcpma<0.01), where only one is expected by chance. These SNPs are therefore candidate drivers for the shared genetic architecture between diseases. The SNPs shown in the lower panel also have strong evidence of association in opposite directions across phenotypes and may be crucial decision points in pathogenesis. Aj = major allele; Am = minor allele. Z scores are reported from published GWA studies and arbitrarily signed relative to the direction of effect in celiac disease. Note that no MS data were available for rs2082412 as it had not been imputed accurately in the participating MS study. Data for all SNPs is presented in Dataset S1. Although our CPMA statistic is agnostic to effect direction in each disease, a subset of the 47 multi-phenotype (CPMA positive) SNPs appeared to have strong allelic effects in opposite directions in different diseases [16]. A total of 9 SNPs had strong evidence of such directional association (an association p<1×10−4 with at least one protective and one risk effect; lower panel in Table 2). This suggests that shared associations have complex effects on disease outcomes and may be of particular importance in pathogenic processes.
We next examined the patterns of association across 47 multi-phenotype SNPs to determine evidence of either a global autoimmune process or biological pathways influencing sets of diseases. On visual inspection of these data we found a striking patterning of associations across diseases: only one SNP (rs3184504, in an exon of SH2B3) exhibited evidence of association to all seven diseases; the others appeared to associate only to subsets of diseases (Table 2).
To formalize the analysis of association patterns across diseases, we determined specific patterns of associations across SNPs by computing SNP-SNP distances based on the level of association to each disease followed by hierarchical clustering to group them (Figure 1A; see Materials and Methods section for clustering details). SNPs in loci encoding proteins known to interact clustered together: for example, the independent effects at IL12B and IL23R, which encode subunits of a ligand-receptor pair are in the same region of the dendrogram. We next partitioned the dendrogram “tree” into four clusters and summarized the cumulative association of each cluster to each disease by combining our underlying dataset of association p-values per cluster, per disease using Fisher's omnibus test (Figure 1B; see Materials and Methods for details). Each cluster had a different pattern of associations across diseases; these patterns suggest that the clusters represent distinct co-morbid mechanisms.
Fig. 1. Patterns of association across diseases correlate with protein-protein interactions. 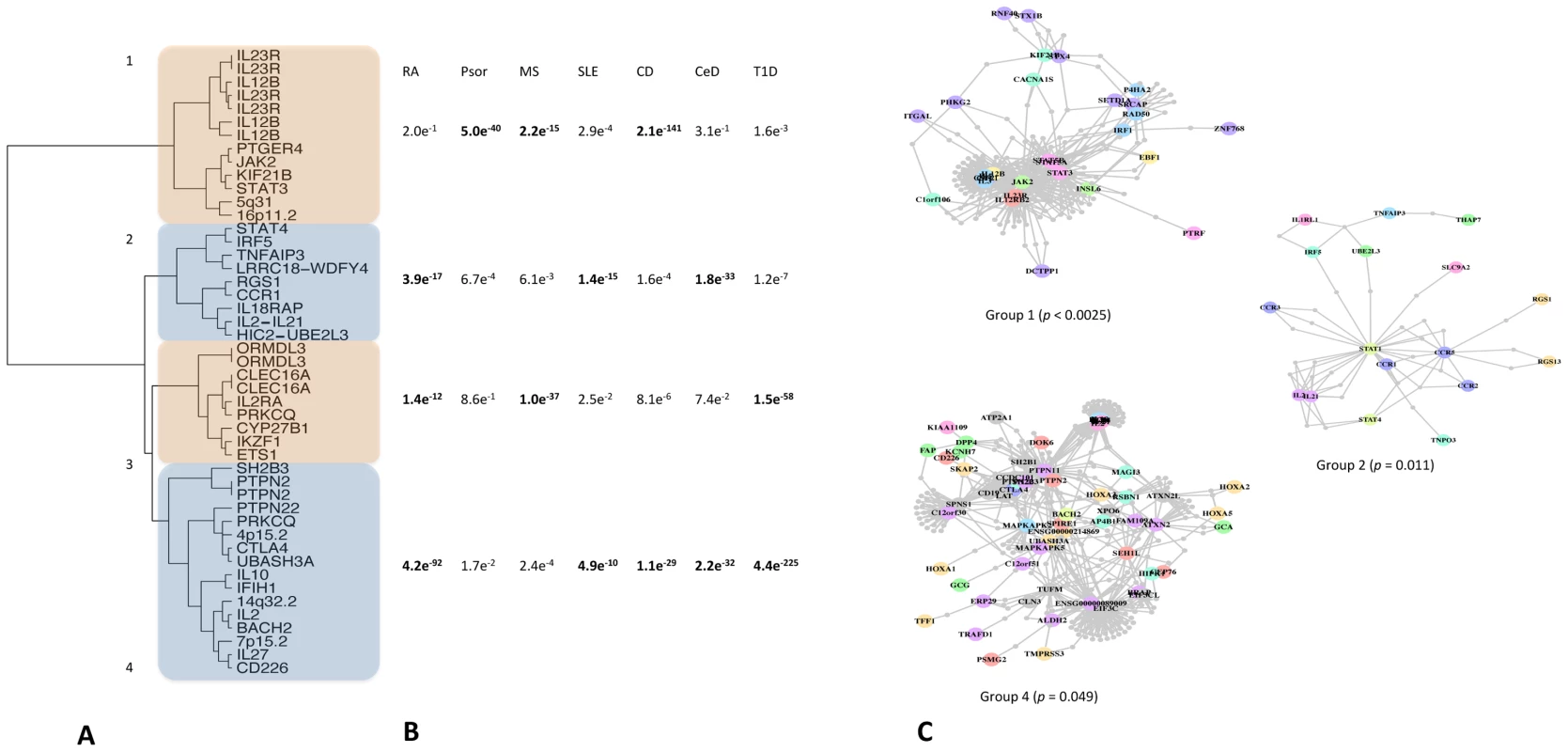
A: 47 SNPs with evidence of association to multiple diseases (Pcpma<0.01) fall into groups clustered by the pattern of association across diseases. Clusters are numbered arbitrarily. B: Clusters show different patterns of association across diseases. We summarize the differential disease effects of each cluster with a cumulative association statistic (Fisher's method for combining p values). These patterns are different for each cluster, suggesting each represents a different co-morbid mechanism. Note that these figures are based on the same underlying association statistics the clustering in the first panel is derived from. C: proteins encoded within the linkage disequilibrium scope around SNPs in the same cluster interact either directly or via common intermediates. Three of our four clusters have significant protein inter-connectivity (permuted P<0.05; see Materials and Methods and [19] for details). Our underlying hypothesis has been that phenotype-driven clusters represent distinct molecular mechanisms. This leads to the prediction that components of these clusters/pathways are encoded in associated loci; in other words, proteins encoded around SNPs in the same cluster should interact. We test this prediction by looking for connectivity between proteins encoded around SNPs within each cluster as described elsewhere [19]. Briefly, we define a genomic region around each SNP in terms of linkage disequilibrium and consider any protein overlapping that region. We then ask if proteins encoded around SNPs in the same cluster interact using protein-protein interaction maps, excluding interactions between proteins in the same region (see Materials and Methods and [19]). We find that three of the four clusters we define by patterns of association have significant connectivity (Figure 1C; permuted P<0.05) by this method, suggesting that these represent distinct molecular mechanisms affected by genetic risk variants. Two of these groups of interacting proteins are also preferentially expressed [19] in immune cell subtypes compared to other tissue types (Figure S1), supporting our hypothesis that these represent true pathways underlying pathogenesis.
Discussion
Immune-mediated inflammatory and autoimmune diseases have been known to cluster in families, suggesting a strong genetic component to risk. The genes in the human MHC (HLA complex) have been associated with disease risk, suggesting a common immune pathway. Less clear is whether other genetic variants associated with individual diseases also form common pathways/mechanisms for autoimmunity. Recent results from GWA studies suggest that common genetic mechanisms may underlie the observed clustering of multiple autoimmune diseases within a person or family. In this work we have tested the hypothesis that immunologically relevant genetic variation will either (1) underlie risk to all immune-mediated diseases, implicating a global immunological process; (2) influence risk to a discrete subset of diseases, implicating molecular entities underlying that co-morbidity; or (3) modulate risk for only one disorder thereby implying a disease-specific process.
A central goal of complex disease genetics is to uncover the pathways perturbed in disease and shed light on the underlying cellular processes. Despite a wealth of molecular insight into immune function few key pathways underlying genetic susceptibility to immune-mediated diseases have been elucidated. To identify these processes in immune-mediated inflammatory and autoimmune disease, we tested genetic variation contributing to seven diseases. We observed an overwhelming abundance of commonality across these phenotypes, assorting into cohesive phenotype-genotype groups that appear to underlie co-morbidities. By analyzing loci known to associate to at least one disease, we are able to identify groups of diseases that should be considered as a unified phenotype and analyzed together. We further demonstrate that this approach generates novel biological insights into pathogenesis, often difficult to obtain from genomic studies of single traits [20].
We have described a novel statistic, CPMA, which assesses evidence for multiple associations to a marker. Rather than perform a meta-analysis, which would only detect association to all phenotypes (or suffer from heterogeneity) or test all combinations of phenotypes which would increase the multiple testing burden, we look for deviation in the distribution of association p values. Our statistic thus detects markers associated to at least some, but not necessarily all, phenotypes; we note that this is a single degree of freedom test, providing high power to reject the null hypothesis. This power comes at the price of not knowing to which phenotypes the marker is associate; we overcome this with our clustering analysis, which resolves groups of markers associating to the same diseases. Thus our analytic strategy is able to both detect shared associations and identify the relevant phenotypes.
Our approach appears capable of distinguishing distinct genetic effects in the same locus in addition to validated shared associations. For example, it is now clear that the two signals in the IL2/IL21 locus on chromosome 4q27 are distinct, with T1D mapping to IL2 and other diseases to IL21 [21]. Our analysis detects this difference, clustering the two SNPs representing these associations separately (Figure 1, labeled “IL2” and “IL2/IL21”, respectively). Conversely, previous reports of an overlap in association between T1D and celiac disease [15] were in regions encoding genes highly expressed in T lymphocytes (RGS1, PTPN2 and CTLA4 in celiac; PTPN2 and CTLA4 in T1D). Our analysis identifies all these regions as CPMA-positive and highlights the second associations in T1D and celiac shown by Smyth et al.[15], indicating that our approach could be used to prioritize marginal associations for replication. We also observe other potential associations. For example, rs2816316 on near RGS1 exhibits evidence of association to MS; rs2542151 and rs1893217 on near PTPN2 has modest association to psoriasis. These last observations, whilst suggestive, require further investigation given the known effects of these regions on other diseases.
In summary, our multi-disease approach is applicable beyond the immune-mediated inflammatory and autoimmune diseases, to current studies of related traits in pharmacology, metabolic and psychiatric disease and in genetic studies of cellular phenotypes such as gene expression. For most studies of the genetic basis of complex human phenotypes, the pathogenic processes are still far from understood and biological pathways may be identified using these methods. Ultimately, these results will contribute to an improved molecular nosology of mechanistic definitions and, ultimately, towards improving clinical care and human health.
Materials and Methods
Ethics statement
All data were drawn from previously published genome-wide association studies from consortia with appropriate ethics oversight from their respective institutional review boards. As only summary data from a small number of markers across the genome were used here no further ethical issues arise.
Patient cohorts
Data were obtained from previously described case/control GWA studies of celiac disease [22], Crohn's disease [2], multiple sclerosis [5], psoriasis [6], rheumatoid arthritis [7], systemic lupus erythematosus [23] and type I diabetes [24] as shown in Table 1. We note that, with the exception of psoriasis, in these cohorts diagnosis of a second immune-mediated disease is a criterion for exclusion, thereby minimizing co-morbidity as a source of bias in our study.
Locus selection
For our analysis we selected 140 independent SNPs (r2<0.2) with reported associations to an immune-mediated disease in a genome-wide association scan and replicated in independent samples in that disease to combined genome-wide significance [25]. We then chose proxies for those SNPs present on the major versions of Affymetrix and Illumina genome-wide genotyping platforms [26]; 107 SNPs had sufficient data coverage to be included. Where possible we used the SNP originally reported; if data were unavailable for that marker, we chose a high LD proxy (HapMap/CEU r2>0.9) to represent the region.
Cross-phenotype meta-analysis
Our CPMA analysis relies on the expected distribution of p-values for each SNP across diseases. Under the null hypothesis of no additional associations beyond those already known, we expect association values to be uniformly distributed and hence -ln(p) to be exponentially decaying with a decay rate λ = 1. We calculate the likelihood of the observed and expected values of λ and express these as a likelihood ratio test:
This statistic therefore measures the likelihood of the null hypothesis given the data; we can reject the null hypothesis if sufficient evidence to the contrary is present. We note that, because we only estimate a single parameter, our test is asymptotically distributed as . This gives us more statistical power than relying on strategies combining association statistics, which would consume multiple degrees of freedom.
SNP–SNP distance calculation and clustering
To compare the patterns of association for multi-phenotype SNPs we first calculate SNP-SNP distances and then use hierarchical clustering on that distance matrix to assess relative relationships between SNP association patterns.
Calculating distances based directly on p values or the underlying association statistics is problematic, as each contributing study has slightly different sample sizes and therefore different statistical power to detect associations. Thus, distance functions based on numeric data – which incorporate magnitude differences between observations – would be biased if studies have systematically different data. Normalization procedures can account for such systematic differences but may fail to remove all bias. To reduce the impact such systematic irregularities might have on our comparison, we bin associations into informal “levels of evidence” categories. We define four classes (1<p<0.05, 0.05<p<0.001, 0.001<p<1×10-6, 1×10−6<p) and thus reduce our data to a SNP x disease matrix where entries are categorical variables describing these classes. We then calculate the Euclidean distances between pairs of SNPs using Gower's method for categorical data [27], which accounts for the discrete nature of the data.
To compare the distance relationships between SNPs we use hierarchical agglomerative clustering. This process joins single entities (in this case, SNPs) or groups of entities together if certain criteria are met. Successive rounds of clustering are preformed in an iterative way until all groups are joined, resulting in a tree of relationships where similar entities cluster on the same branches. In this analysis we cluster SNPs based on the Gower distance matrix using Ward's method for joining entities [28]. In contrast to linkage clustering methods, Ward's method seeks to minimize the information lost during the clustering process, calculated as the error sum of squares (ESS). The higher the ESS the more information is being lost due to inaccuracy of grouping entities together. This method thus seeks compact, spherical clusters of data which are maximally similar.
All distance and clustering analysis was done using the StatMatch and stats packages in the R programming language [29].
Cumulative association statistics
We compute per-cluster, per-disease cumulative association statistics by combining p values using Fisher's omnibus test, where the cumulative statistic Scum on N p-values is defined as:
and Scum follows the distribution with 2N degrees of freedom.
Protein–protein interaction analysis
We use previously described methodology [19] to assess whether proteins encoded around SNPs in each cluster interact. Briefly, we first compile lists of all proteins that an association may affect by defining locus boundaries around each SNP in terms of linkage disequilibrium and including all proteins overlapping this region. We then use a high-confidence protein-protein interaction map ([30] as modified in [19]) to ask whether proteins encoded around SNPs in each cluster interact either directly or via a common intermediary and assess the significance of such observations relative to the local structure of the protein-protein network as described elsewhere [19], using 4000 permutations. These data and methodology are publicly available for download and via a webserver (http://www.broadinstitute.org/mpg/dapple).
Supporting Information
Zdroje
1. VyseTToddJ 1996 Genetic analysis of autoimmune disease. Cell 85 311 318
2. BarrettJCHansoulSNicolaeDChoJDuerrRH 2008 Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease. Nat Genet 40 955 962
3. GrahamRCotsapasCDaviesLHackettR 2008 Genetic variants near TNFAIP3 on 6q23 are associated with systemic lupus erythematosus. Nat Genet 40 1059 1061
4. HuntKAZhernakovaATurnerGHeapGARFrankeL 2008 Newly identified genetic risk variants for celiac disease related to the immune response. Nat Genet 40 395 402
5. De JagerPLJiaXWangJDe BakkerPIWdOttoboniL 2009 Meta-analysis of genome scans and replication identify CD6, IRF8 and TNFRSF1A as new multiple sclerosis susceptibility loci. Nat Genet 41 776
6. NairRPDuffinKCHelmsCDingJStuartPE 2009 Genome-wide scan reveals association of psoriasis with IL-23 and NF-κB pathways. Nat Genet 41 199 204
7. StahlEARaychaudhuriSRemmersEFXieGEyreS 2010 Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat Genet 42 508 514
8. CriswellLPfeifferKLumRGonzalesBNovitzkeJ 2005 Analysis of families in the multiple autoimmune disease genetics consortium (MADGC) collection: the PTPN22 620W allele associates with multiple autoimmune phenotypes. The American Journal of Human Genetics 76 561 571
9. WandstratAWakelandE 2001 The genetics of complex autoimmune diseases: non-MHC susceptibility genes. Nature immunology 2 802 809
10. EatonWRoseNKalaydjianAPedersenMMortensenP 2007 Epidemiology of autoimmune diseases in Denmark. Journal of Autoimmunity 29 1 9
11. MaierLLoweCCooperJDownesKAndersonD 2009 IL2RA genetic heterogeneity in multiple sclerosis and type 1 diabetes susceptibility and soluble interleukin-2 receptor production. PLoS Genet 5 e1000322 doi:10.1371/journal.pgen.1000322
12. PlengeRMCotsapasCDaviesLPriceALDe BakkerPIWd 2007 Two independent alleles at 6q23 associated with risk of rheumatoid arthritis. Nat Genet 39 1477 1482
13. RemmersEFPlengeRMLeeATGrahamRHomG 2007 STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. The New England Journal of Medicine 357 977 986
14. FungEYSmythDJHowsonJMCooperJDWalkerNM 2009 Analysis of 17 autoimmune disease-associated variants in type 1 diabetes identifies 6q23/TNFAIP3 as a susceptibility locus. Genes Immun 10 188 191
15. SmythDJPlagnolVWalkerNMCooperJDDownesK 2008 Shared and distinct genetic variants in type 1 diabetes and celiac disease. The New England Journal of Medicine 359 2767 2777
16. SirotaMSchaubMABatzoglouSRobinsonWHButteAJ 2009 Autoimmune disease classification by inverse association with SNP alleles. PLoS Genet 5 e1000792 doi:10.1371/journal.pgen.1000792
17. ZhernakovaAvan DiemenCWijmengaC 2009 Detecting shared pathogenesis from the shared genetics of immune-related diseases. Nat Rev Genet 10 43 55
18. de BakkerPIWdMcveanGSabetiPCMirettiMMGreenT 2006 A high-resolution HLA and SNP haplotype map for disease association studies in the extended human MHC. Nat Genet 38 1166 1172
19. RossinELageKRaychaudhuriSXavierRTatarD 2011 Proteins Encoded in Genomic Regions Associated with Immune-Mediated Disease Physically Interact and Suggest Underlying Biology. PLoS Genet 7 e1001273 doi:10.1371/journal.pgen.1001273
20. KhannaHDavisEEMurga-ZamalloaCAEstrada-CuzcanoALopezI 2009 A common allele in RPGRIP1L is a modifier of retinal degeneration in ciliopathies. Nat Genet 41 739 745
21. ToddJA 2010 Etiology of type 1 diabetes. Immunity 32 457 467
22. DuboisPCATrynkaGFrankeLHuntKARomanosJ 2010 Multiple common variants for celiac disease influencing immune gene expression. Nature Publishing Group 42 295 302
23. GatevaVSandlingJKHomGTaylorKEChungSA 2009 A large-scale replication study identifies TNIP1, PRDM1, JAZF1, UHRF1BP1 and IL10 as risk loci for systematic lupus erythematosus. Nat Genet 41 1228 1233
24. BarrettJCClaytonDGConcannonPAkolkarBCooperJD 2009 Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet 41 703
25. HindorffLSethupathyPJunkinsHRamosEMehtaJ 2009 Potential etiologic and functional implications of genome-wide association loci for human diseases and traits. Proceedings of the National Academy of Sciences 106 9362
26. JohnsonADHandsakerRPulitSNizzariMO'DonnellCJ 2008 SNAP: a web-based tool for identification and annotation of proxy SNPs using HapMap. Bioinformatics 24 2938 2939
27. GowerJ 1971 A general coefficient of similarity and some of its properties. Biometrics 27 857 874
28. WardJJr 1963 Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association 236 244
29. Team RDC 2010 R: A Language and Environment for Statistical Computing. Vienna, Austria
30. LageKKarlbergEOStørlingZMÓlasonPÍPedersenAG 2007 A human phenome-interactome network of protein complexes implicated in genetic disorder. Nat Biotechnol 25 309 316
Štítky
Genetika Reprodukční medicína
Článek The T-Box Factor MLS-1 Requires Groucho Co-Repressor Interaction for Uterine Muscle SpecificationČlánek B Chromosomes Have a Functional Effect on Female Sex Determination in Lake Victoria Cichlid FishesČlánek Distinct Cdk1 Requirements during Single-Strand Annealing, Noncrossover, and Crossover RecombinationČlánek Specification of Corpora Cardiaca Neuroendocrine Cells from Mesoderm Is Regulated by Notch SignalingČlánek Ongoing Phenotypic and Genomic Changes in Experimental Coevolution of RNA Bacteriophage Qβ and
Článek vyšel v časopisePLOS Genetics
Nejčtenější tento týden
2011 Číslo 8
-
Všechny články tohoto čísla
- Polo, Greatwall, and Protein Phosphatase PP2A Jostle for Pole Position
- Genome-Wide Association Analysis of Incident Coronary Heart Disease (CHD) in African Americans: A Short Report
- The T-Box Factor MLS-1 Requires Groucho Co-Repressor Interaction for Uterine Muscle Specification
- B Chromosomes Have a Functional Effect on Female Sex Determination in Lake Victoria Cichlid Fishes
- Analysis of DNA Methylation in a Three-Generation Family Reveals Widespread Genetic Influence on Epigenetic Regulation
- PP2A-Twins Is Antagonized by Greatwall and Collaborates with Polo for Cell Cycle Progression and Centrosome Attachment to Nuclei in Drosophila Embryos
- Discovery of Sexual Dimorphisms in Metabolic and Genetic Biomarkers
- Pervasive Sharing of Genetic Effects in Autoimmune Disease
- DNA Methylation and Histone Modifications Regulate Shoot Regeneration in by Modulating Expression and Auxin Signaling
- Mutations in and Reveal That Cartilage Matrix Controls Timing of Endochondral Ossification by Inhibiting Chondrocyte Maturation
- Variance of Gene Expression Identifies Altered Network Constraints in Neurological Disease
- Frequent Beneficial Mutations during Single-Colony Serial Transfer of
- Increased Gene Dosage Affects Genomic Stability Potentially Contributing to 17p13.3 Duplication Syndrome
- Distinct Cdk1 Requirements during Single-Strand Annealing, Noncrossover, and Crossover Recombination
- Hunger Artists: Yeast Adapted to Carbon Limitation Show Trade-Offs under Carbon Sufficiency
- Suppression of Scant Identifies Endos as a Substrate of Greatwall Kinase and a Negative Regulator of Protein Phosphatase 2A in Mitosis
- Temporal Dynamics of Host Molecular Responses Differentiate Symptomatic and Asymptomatic Influenza A Infection
- MK2-Dependent p38b Signalling Protects Hindgut Enterocytes against JNK-Induced Apoptosis under Chronic Stress
- Specification of Corpora Cardiaca Neuroendocrine Cells from Mesoderm Is Regulated by Notch Signaling
- Genome-Wide Gene-Environment Study Identifies Glutamate Receptor Gene as a Parkinson's Disease Modifier Gene via Interaction with Coffee
- Identification of Functional Toxin/Immunity Genes Linked to Contact-Dependent Growth Inhibition (CDI) and Rearrangement Hotspot (Rhs) Systems
- Genomic Analysis of the Necrotrophic Fungal Pathogens and
- Celsr3 Is Required for Normal Development of GABA Circuits in the Inner Retina
- Genetic Architecture of Aluminum Tolerance in Rice () Determined through Genome-Wide Association Analysis and QTL Mapping
- Predisposition to Cancer Caused by Genetic and Functional Defects of Mammalian
- Regulation of p53/CEP-1–Dependent Germ Cell Apoptosis by Ras/MAPK Signaling
- and but Not Interact in Genetic Models of Amyotrophic Lateral Sclerosis
- Gamma-Tubulin Is Required for Bipolar Spindle Assembly and for Proper Kinetochore Microtubule Attachments during Prometaphase I in Oocytes
- Ongoing Phenotypic and Genomic Changes in Experimental Coevolution of RNA Bacteriophage Qβ and
- Genetic Architecture of a Reinforced, Postmating, Reproductive Isolation Barrier between Species Indicates Evolution via Natural Selection
- -eQTLs Reveal That Independent Genetic Variants Associated with a Complex Phenotype Converge on Intermediate Genes, with a Major Role for the HLA
- The GATA Factor ELT-1 Works through the Cell Proliferation Regulator BRO-1 and the Fusogen EFF-1 to Maintain the Seam Stem-Like Fate
- and Control Optic Cup Regeneration in a Prototypic Eye
- A Comprehensive Map of Mobile Element Insertion Polymorphisms in Humans
- An EMT–Driven Alternative Splicing Program Occurs in Human Breast Cancer and Modulates Cellular Phenotype
- Evidence for Hitchhiking of Deleterious Mutations within the Human Genome
- A Broad Brush, Global Overview of Bacterial Sexuality
- Global Chromosomal Structural Instability in a Subpopulation of Starving Cells
- A Pre-mRNA–Associating Factor Links Endogenous siRNAs to Chromatin Regulation
- Glutamine Synthetase Is a Genetic Determinant of Cell Type–Specific Glutamine Independence in Breast Epithelia
- The Repertoire of ICE in Prokaryotes Underscores the Unity, Diversity, and Ubiquity of Conjugation
- Genome-Wide Association Analysis of Autoantibody Positivity in Type 1 Diabetes Cases
- Natural Polymorphism in BUL2 Links Cellular Amino Acid Availability with Chronological Aging and Telomere Maintenance in Yeast
- Chromosome Painting Reveals Asynaptic Full Alignment of Homologs and HIM-8–Dependent Remodeling of Chromosome Territories during Meiosis
- Ku Must Load Directly onto the Chromosome End in Order to Mediate Its Telomeric Functions
- PLOS Genetics
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- An EMT–Driven Alternative Splicing Program Occurs in Human Breast Cancer and Modulates Cellular Phenotype
- Chromosome Painting Reveals Asynaptic Full Alignment of Homologs and HIM-8–Dependent Remodeling of Chromosome Territories during Meiosis
- Discovery of Sexual Dimorphisms in Metabolic and Genetic Biomarkers
- Regulation of p53/CEP-1–Dependent Germ Cell Apoptosis by Ras/MAPK Signaling
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Současné možnosti léčby obezity
nový kurzAutoři: MUDr. Martin Hrubý
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



